Abstract
Ventricular fibrillation (VF) is one of the most life threatening events. Although in humans VF is generally sustained (SVF) requiring artificial defibrillation, in various mammals and in some cases in humans VF terminates by itself, reverting spontaneously into sinus rhythm. Since VF is one of the main causes of sudden death, one of the important clinical problems today is if and how we can transform the fatal SVF into a self limited transient one (TVF).
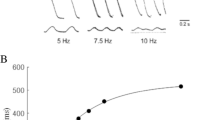
From electrophysiological studies carried out on anaesthetized open chest animals, we have found that TVF requires a high degree of intercellular coupling and synchronization.
Cardiac myocytes are electrically coupled with adjacent cells. The intercellular coupling is a focus of low electrical resistance which allows rapid transmission of electrical impulses between cells. Any decrease in intercellular coupling decreases the ability of the heart for self defibrillation. The cell-to-cell coupling decreases with age, ischemia, VF and variations in physiological conditions probably due to an increase in intercellular resistance (Ri), widening in the internexal gaps, decrease in electrotonic space constant (λ) etc. All of these factors are known to be affected by intracellular concentration of free Ca++ ([Ca++]).
On the basis of studies carried out on various mammals at different ages, we hypothesized that the ability of the heart to defibrillate depends on the cardiac catecholamine level [CA], during VF. This hypothesis is supported by the facts, known from the literature, that increase in [CA] decreases intracellular free Ca++ concentration, decreases Ri and increases λ. By these effects, increase in [CA] enhances intercellular coupling and intercellular synchronization, and thereby, according to our hypothesis, leads to spontaneous ventricular defibrillation — TVF.
During VF the sympathetic activity is enhanced but in some cases the [CA] does not reach the level needed for TVF. In order to help the heart in its effort to elevate the [CA] during VF, we proposed to treat these cases with drugs which inhibit the reuptake of [CA]. The facts that administration of [CA] reuptake inhibitors, before the induction of VF, and/or intracoronary infusion of adrenaline, during VF, transforms SVF into TVF, emphasized the validity of our hypothesis.
Similar content being viewed by others
References
Wigers CJ: Studies of ventricular fibrillation caused by electrical shock. Am Heart J 5: 351–365, 1929
Wigers CJ: The mechanism and nature of ventricular fibrillation. Am Heart J 20: 399–412, 1940
Bacaner M: Experimental and clinical effects of bretylium tosylate on ventricular fibrillation, arrhythmias and heart block. Geriatrics 26: 132–148, 1971
Zipes DP, Fisher J, King RM, Nicoll AB, Jolly WW: Termination of ventricular fibrillation in dogs by depolarizating a critical amount of myocardium. Am J Cardiol 36: 37–44, 1975
Damiano RJ, Asano T, Smith PK, Cox JL: Effect of the right ventricular isolation procedure on ventricular vulnerability to fibrillation. J Am Coll Cardiol 15: 730–736, 1990
Watanabe Y: Antifibrillatory action of several antiarrhythmic agents. In: S. Hayase and S. Murao (eds). Cardiology. Proceedings of 8th World Congress of Cardiology. Excerpta Medica, Amsterdam, 1979, pp 924–928
West TC, Landa JF: Minimal mass required for induction of a sustained arrhythmias in isolated atrial segments. Am J Physiol 202: 232–236, 1962
Manoach M, Varon D, Neuman M, Netz H: Spontaneous termination and initiation of ventricular fibrillation as a function of heart size, age, autonomic autoregulation and drugs: A comparative study on different species of different age. Heart and Vessels 2 (Suppl): 56–68, 1987
Manoach M, Netz H, Erez M, Weinstock M: Ventricular self defibrillation in mammals: age and drug dependence. Age and Ageing 9: 112–116, 1980
Schwartz SP, Orloff J, Fox C: Transient ventricular fibrillation. Am Heart J 37: 21–35, 1949
Goble AJ: Paroxysmal ventricular fibrillation with spontaneous reversion to sinus rhythm. Brt Heart J 27: 62–68, 1965
Spielman SR, Farshidi A, Horowitz LN, Josephson ME: Ventricular fibrillation during programmed ventricular stimulation incidence and clinical implications. Am J Cardiol 42: 913–918, 1978
Patt MV, Podrid PJ, Friedman PL, Lown B: Spontaneous reversion of ventricular fibrillation. Am Heart J 115: 919–923, 1988
Clayton R, Higham D, Murray A, Campell R: Self terminating ventricular fibrillation. (Abs) J Am Coll Cardiol 19: 265A, 1992
Kobrin VI, Kudinova ED: Electrical activity of intact myocardial cells in different animals during normal activity and ventricular fibrillation. In: Proceedings of the international symposium on problems in comparative electrophysiology. Syktivkar, USSR, 1979, p 36 (abst)
Dessertenne F: La tachycardie ventriculaire a deux foyers opposes variables. Arch Mal Coeur 59: 263–272, 1966
Krikler DM, Curry PLV: Torsade de pointes, an atypical ventricular tachycardia. Br Heart J 38: 117–120, 1976
Ranquin R, Parizel G: Ventricular fibrillo-flutter. Torsade de pointes; an established electrocardiographic and clinical entity. Angiology 28: 115–118, 1977
Sclarovsky S, Strasberg B, Levin R, Agmon J: Polymorphous ventricular tachycardia: clinical features and treatment. Am J Cardiol 44: 339–344, 1979
Selzer A, Wray HW: Quinidine syncope. Paroxysmal ventricular fibrillation occuring during treatment of chronic atrial arrhythmias. Cir Res 25: 17–26, 1964
Bacaner M: Bretylium tosylate for suppression of induced ventricular fibrillation. Am J Cardiol 17: 528–534, 1966
Sanna G, Archidiacono R: Chemical ventricular defibrillation of the human heart with bretylium tosylate. Am J Cardiol 32: 982–986, 1973
Manoach M, Netz H, Varon D, Amitzur G, Weinstock M, Kauli N, Assael M: Factors influencing spontaneous initiation and termination of ventricular fibrillation. Jap Heart J 27: 365–375, 1986
Manoach M, Beker B, Erez M, Varon D, Netz H: Spontaneous termination of electrically induced ventricular fibrillation. In: P.W. Mecfarlane (ed.). Progress in electrocardiology. Pitman Med Pub, England, 1979, pp 361–365
Manoach M, Erez M, Varon D: Editorial review. Properties required for self ventricular fibrillation: Influence of age and drugs. Cardiol in the Elderly 1: 337–344, 1993
Amitzur G, Manoach M, Weinstock M: The influence of cardiac cholinergic activation on the induction and maintenance of ventricular fibrillation. Basic Res Cardiol 79: 690–697, 1984
Manoach M, Netz H, Beker B, Kauli N: Vector-cardiographycal discrimination between sustained and transient ventricular fibrillation. In: F. dePadua and P.W. Macfarlane (eds). New frontiers of electrocardiology. Research studies press, J Wiley and Sons, England, 1981, pp 139–143
Chen-Menaker A, Einav S, Manoach M: Signal processing of the ECG during ventricular fibrillation. In: Proceedings IEEE Conv, Haifa, Israel, 1985, 2.4,6: 1–3
Manoach M, Wyatt RF: Intracellular myocardial recordingsin vivo during sustained and transient ventricular fibrillation. In: P. d'Alche (ed.). Advances in electrocardiology University of Caen, France, 1985, pp 401–403
Manoach M, Kauli N, Pinchasov A, Beker B, Netz H, Varon D: Electrical and mechanical differences between sustained and transient ventricular fibrillation (abst). Israel J Med Sc 16: 225, 1980
Spach MS, Miller WT, Geselowitz DB, Barr RC, Kootsey JM, Johnson EA: The discontinuous nature of propagation in normal canine cardiac muscle. Cir Res 48: 39–54, 1981
Bredikis J, Bukaskas F, Veteikis R: Decreased intercellular coupling after prolonged rapid stimulation in rabbit atrial muscle. Cir Res 49: 815–820, 1981
Arnsdorf ME: Membrane factors in arrhythmogenesis: Concepts and definitions. Prog Cardiovas Dis 19: 413–429, 1977
Spach MS, Kootsey JM, Sloan JD: Active modulation of electrical coupling between cardiac cells of the dog. Cir Res 51: 347–362, 1982
De Mello WC: Increased spread of electrotonic potentials during diastolic depolarization in cardiac muscle. J Mol Cell Cardiol 18: 23–29, 1986
Kukushkin NI, Bukauskas FF, Sakson ME, Nasokoya VV: Anisotropy of stationary velocity and delaye of extrasystole waves in the dog heart. Biofizika 20: 687–692, 1975
De Mello WC: Cell-to-cell coupling assayed by means of electrical measurements. Experientia 43: 1075–1079, 1987
Weingart R, Maurer P: Cell-to-cell coupling studied in isolated ventricular cell pairs. Experientia 43: 1091–10994, 1987
Liberman M, Kootsey JM, Johnson EA, Sawanobori T: Slow conduction in cardiac muscle. Biophys J 13: 37–55, 1973
Delese J: Cell to cell communication in the heart: structure function correlations. Experientia 43: 1068–1075, 1987
Wojtezak J: Contractures and increase in internal longitudinal resistance of cow ventricular muscle induced by hypoxia. Cir Res 44: 88–95, 1979
Weingart R: The action of ouabain on intercellular coupling and conduction velocity in mammalian ventricular muscle. J Phisiol (Lond) 264: 341–365, 1977
Chen CM, Gettes LS: Combined effect of rate, membrane potential and drug on maximal rate of rise (Vmax) of action-potential upstroke of guinea pig papillary muscle. Cir Res 38: 464–469, 1976
Sano T: Mechanism of cardiac fibrillation. Pharmacol Ther 2: 407–513, 1976
De Mello WC: Effect of intracellular injection of calcium and strontium on cell communication in heart. J Physiol (Lond) 250: 231–245, 1975
De Mello WC: Influence of the sodium pump on intercellular communication in heart fibers: effect of intracellular injection of sodium ion on electrical coupling. J Physiol (Lond) 263: 171–197, 1976
Burt JM, Spray DC: Adrenergic control of gap junction conductance in cardiac myocytes (abst). Circulation 78: Suppl II, 258, 1988
Lamont SV, Barritt GJ: Effects of Adrenaline on a compartment of slowly-exchangeable Ca in the perfused rat heart. Cardiovas Research 17: 88–95, 1982
Entman ML, Levey GS, Epstein SE: Mechanism of action of epinephrine and glucagon on the canine heart. Evidence for increase in sarcotubular calcium stores mediated by cyclic 3′, 5′ AMP. Cir Res 25: 429–438, 1969
Li T, Vassalle M: The negative inotropic effect of calcium overload in cardiac Purkije fibers. J Mol Cell Cardiol 16: 65–77, 1984
Manoach M, Varon D, Erez M: A self-protecting servo-mechanism involved in spontaneous ventricular defibrillation. J Basic and Clin Physiol and Pharmacol 4: 273–280, 1993
Eisenhofer G, Esler MD, Cox HS, Meredith IT, Jennings GL, Brush JE Jr, Goldstein DS: Differences in the neronal removal of circulating epinephrine and norepinephrine. J Clin Endocrinol Metab 70: 1710–1720, 1990
Goldstein DS, Brush JE Jr, Eisenhofer G, Stull R, Elser M:In vivo measurement of neuronal uptake of norepinephrine in the human heart. Circulation 78: 41–48, 1988
Spadary RC, De-Moraes S: Aging and rat pacemaker sensitivity to beta adrenoceptor agonists. Braz J Med Biol Res 20: 591–594, 1987
Daly RN, Goldberg PB, Roberts J: The effect of age on presynaptic alpha2 adrenoceptor autoregulation of norepinephrine release. J Gerontol 44: 859–866, 1989
Fleisch JH: Age related decrease in both adrenoceptor activity of the cardiovascular system. Treads Pharmacol Sci 2: 337–339, 1981
Abrass IB, Davis JL, Searpace PJ: Isoproterenol responsiveness and myocardial beta adrenergic receptors in young and old rats. J Gerentol 37: 156–160, 1982
Manoach M, Varon D, Neuman M, Erez M: Minireview. The cardioprotective features of tricyclic antidepressants. Gen Pharmac 20: 269–275, 1988
Manoach M, Erez M, Wozner D, Varon D: Ventricular defibrillating properties of catecholamine uptake inhibitors. Life Sc 51: PL 159–164, 1992
Manoach M, Tager S, Erez M, Varon D, Vaugham Williams M: The defibrillating effect of high cardiac catecholamine level. (Abst) J Moll Cell Cardiol 24: Supp V, S69, 1992
Lombardy F, Verrier RL, Lown B: Relationship between sympathetic neural activity, coronary dynamics and vulnerability to ventricular fibrillation during myocardial ischemia and reperfision. Am Heart J 105: 958–965, 1983
Jones DL, Klein GL: Ventricular fibrillation: The importance to be course. J Electrocardiol 17: 393–399, 1984
Wagner GS, McIntosh HD: The use of drugs in achieving successful DC cardioversion. Prog Cardiovasc Dis 11: 431–442, 1969
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Manoach, M., Varon, D. & Erez, M. The role of catecholamines on intercellular coupling, myocardial cell synchronization and self ventricular defibrillation. Mol Cell Biochem 147, 181–185 (1995). https://doi.org/10.1007/BF00944799
Issue Date:
DOI: https://doi.org/10.1007/BF00944799