Abstract
Background/Objectives. A rapid diagnosis of ST-segment elevation myocardial infarction (STEMI) is mandatory for optimal treatment. However, a small proportion of patients with suspected STEMI suffer from other conditions. Although case reports have described these conditions, a contemporary systematic analysis is lacking. We report the incidence, clinical characteristics and outcome of patients with suspected STEMI referred for primary percutaneous coronary intervention (PCI) with a final diagnosis other than STEMI.
Methods. From January 2004 to July 2005, 820 consecutive patients were included with suspected STEMI who were referred for primary PCI to a university medical centre, based on a predefined protocol. Clinical characteristics, final diagnosis and outcome were obtained from patient charts and databases.
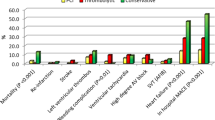
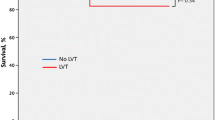
Results. In 19 patients (2.3%), a final diagnosis other than myocardial infarction was established: coronary aneurysm (n=1), (myo)pericarditis (n=5), cardiomyopathy (n=2), Brugada syndrome (n=1), aortic stenosis (n=1), aortic dissection (n=3), subarachnoidal haemorrhage (n=2), pneumonia (n=1), chronic obstructive pulmonary disease (n=1), mediastinal tumour (n=1), and peritonitis after recent abdominal surgery (n=1). These patients less often reported previous symptoms of angina (p<0.001), smoking (p<0.05) and a positive family history of cardiovascular diseases (p<0.05) than STEMI patients. Mortality at 30 days was 16%.
Conclusion. A 2.3% incidence of conditions mimicking STEMI was found in patients referred for primary PCI. A high clinical suspicion of conditions mimicking STEMI remains necessary. (Neth Heart J 2008;16:325-31.)
Similar content being viewed by others
References
Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 2006;355:2308-20.
Brodie BR, Stuckey TD, Wall TC, et al. Importance of time to reperfusion for 30-day and late survival and recovery of left ventricular function after primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 1998;32:1312-9.
Zijlstra F, Patel A, Jones M, et al. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2-4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J 2002;23:550-7.
DeWood MA, Spores J, Notske R, et al. Prevalence of total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Med 1980;303:897-902.
Widimsky P, Stellova B, Groch L, et al. Prevalence of normal coronary angiography in the acute phase of suspected ST-elevation myocardial infarction: experience from the PRAGUE studies. Can J Cardiol 2006;22:1147-52.
Da Costa A, Isaaz K, Faure E, Mourot S, Cerisier A, Lamaud M. Clinical characteristics, aetiological factors and long-term prognosis of myocardial infarction with an absolutely normal coronary angiogram; a 3-year follow-up study of 91 patients. Eur Heart J 2001;22:1459-65.
Raymond R, Lynch J, Underwood D, Leatherman J, Razavi M. Myocardial infarction and normal coronary arteriography: a 10 year clinical and risk analysis of 74 patients. J Am Coll Cardiol 1988; 11:471-7.
Wang K, Asinger RW, Marriott HJ. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003; 349:2128-35.
Bertrand ME, Simoons ML, Fox KA, et al. Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2002;23:1809-40.
Angelini A, Calzolari V, Calabrese F, et al. Myocarditis mimicking acute myocardial infarction: role of endomyocardial biopsy in the differential diagnosis. Heart 2000;84:245-50.
Surawicz B, Lasseter KC. Electrocardiogram in pericarditis. Am J Cardiol 1970;26:471-4.
Livaditis IG, Paraschos M, Dimopoulos K. Massive pulmonary embolism with ST elevation in leads V1-V3 and successful thrombo-lysis with tenecteplase. Heart 2004;90:e41.
Spittell PC, Spittell JA Jr, Joyce JW, et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990). Mayo Clin Proc 1993;68:642-51.
Ryan ET, Pak PH, DeSanctis RW. Myocardial infarction mimicked by acute cholecystitis. Ann Intern Med 1992;116:218-20.
Fulton MC, Marriott HJ. Acute pancreatitis simulating myocardial infarction in the electrocardiogram. Ann Intern Med 1963;59: 730-2.
Bouten MJ, Simoons ML. Strategies for pre-hospital thrombo-lysis: an overview. Eur Heart J 1991;12 (Suppl G):39-42.
Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 1992;20:1391-6.
Elsman P, Alleman MA, Zijlstra F. [Clinical presentations mimicking acute myocardial infarction; therapeutic pitfalls]. Ned Tijd-schr Geneeskd 1998;142:1057-60.
Costantini M,Tritto C, Licci E, et al. Myocarditis with ST-Elevation Myocardial Infarction presentation in young man. A case series of 11 patients. Int J Cardiol 2005;101:157-8.
Ozeke O, Aras D, Deveci B, Yildiz A, Maden O, Selcuk MT. Brugada-like early repolarization pattern misdiagnosed as acute anterior myocardial infarction in a patient with myocardial bridging of the left anterior descending artery. Mt Sinai J Med 2006;73: 627-30.
Sajeev CG, Vinayakumar D, Venugopal K. Brugada syndrome simulating acute myocardial infarction. Int J Cardiol 2005;99: 155-6.
Antman EM, Braunwald E. ST-elevation myocardial infarction: pathology, pathophysiology, and clinical features. In: Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's heart disease: a textbook of cardiovascular medicine. Philadelphia, PA: Elsevier Saunders; 2005:1141-65.
Blankenship JC, Almquist AK. Cardiovascular complications of thrombolytic therapy in patients with a mistaken diagnosis of acute myocardial infarction. J Am Coll Cardiol 1989;14:1579-82.
Kahn JK. Inadvertent thrombolytic therapy for cardiovascular diseases masquerading as acute coronary thrombosis. Clin Cardiol 1993;16:67-71.
Gu YL, van den Heuvel AFM, Erasmus ME, Zijlstra F. Aortic dissection presenting as acute myocardial infarction: potential harm of antithrombin and antiplatelet therapy. Neth Heart J 2006;14: 147-9.
Nakamura Y, Kaseno K, Kubo T. Transient ST-segment elevation in subarachnoid hemorrhage. J Electrocardiol 1989;22:133-7.
Lee TH, Cannon CP. Approach to the patient with chest pain. In: Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's heart disease: a textbook of cardiovascular medicine. Philadelphia, PA: Elsevier Saunders; 2005:1129-39.
Chapman GD, Ohman EM, Topol EJ, et al. Minimizing the risk of inappropriately administering thrombolytic therapy (Thrombolysis and Angioplasty in Myocardial Infarction [TAMI] study group). Am J Cardiol 1993;71:783-7.
Khoury NE, Borzak S, Gokli A, Havstad SL, Smith ST, Jones M. “Inadvertent” thrombolytic administration in patients without myocardial infarction: clinical features and outcome. Ann Emerg Med 1996;28:289-93.
Terkelsen CJ, Lassen JF, Norgaard BL, et al. Reduction of treatment delay in patients with ST-elevation myocardial infarction: impact of pre-hospital diagnosis and direct referral to primary percutaneous coronary intervention. Eur Heart J 2005;26:770-7.
Larson DM, Menssen KM, Johnson RK, et al. False positive ST elevation in patients undergoing direct percutaneous coronary intervention. Circulation 2006;114:II-346.
van 't Hof AW, Rasoul S, van de Wetering H, et al. Feasibility and benefit of prehospital diagnosis, triage, and therapy by paramedics only in patients who are candidates for primary angioplasty for acute myocardial infarction. Am Heart J 2006;151:1255-5.e5.
Author information
Authors and Affiliations
Corresponding author
Additional information
Department of Cardiology, University Medical Center Groningen, University of Groningen, Groningen, the Netherlands
Correspondence to: Y.L. Gu, Department of Cardiology, University Medical Center Groningen, University of Groningen, PO Box 30001, 9700 RB Groningen, the Netherlands
Rights and permissions
About this article
Cite this article
Gu, Y.L., Svilaas, T., van der Horst, I.C.C. et al. Conditions mimicking acute ST-segment elevation myocardial infarction in patients referred for primary percutaneous coronary intervention. NHJL 16, 325–331 (2008). https://doi.org/10.1007/BF03086173
Issue Date:
DOI: https://doi.org/10.1007/BF03086173