Abstract
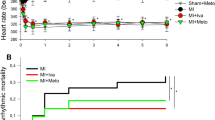
The combination of a calcium antagonist with an angiotensin-converting enzyme (ACE) inhibitor is increasingly used in the therapy of hypertension, but there are no experimental data supporting the use of this combination in acute myocardial ischemia and reperfusion. We tested the effects of oral pretreatment in a pig model, paying special attention to arrhythmias and adverse hemodynamic effects. Pigs received verapamil 240 mg + trandolapril 4 mg, verapamil 240 mg, or placebo orally once daily for 10 days, after which a coronary artery was ligated for 20 minutes and then allowed to reperfuse. The ventricular fibrillation threshold (VFT) was measured during ischemia to assess the vulnerability of the heart to ventricular fibrillation, whereas spontaneous tachyarrhythmias were monitored during reperfusion. Regional left ventricular (LV) blood flow was measured with radioactive microspheres. During the ischemic period, both the combination of verapamil plus trandolapril, and verapamil alone, prevented a fall in the VFT, indicating antiarrhythmic activity. The combination maintained LV contractile activity and cardiac output (CO) at preligation levels, whereas verapamil alone decreased cardiac output. During reperfusion, verapamil plus trandolapril prevented spontaneous ventricular tachyarrhythmias and increased blood flow in the reperfused zone. In contrast, verapamil was not antiarrhythmic and decreased CO. Thus the addition of the ACE inhibitor trandolapril to the calcium antagonist verapamil resulted in antiarrhythmic activity during ischemia and reperfusion, and produced a better hemodynamic profile.
Similar content being viewed by others
References
Rapoport RM, Draznin MB, Murad F. Endothelium-dependent relaxation in rat aorta may be mediated through cyclic GMP dependent protein phosphorylation. Nature 1983; 306:174-176.
Lücsher TF. Angiotensin, ACE inhibitors and endothelial control of vasomotor tone. Basic Res Cardiol 1993;88(Suppl. 1):15-24.
Mancia G, Grassi G. Combination treatment in antihypertensive drug trials. Cardiovasc Drug Ther 1997;11:517-518.
DAVIT I Study. Danish Study Group on Verapamil in Myo cardial Infarction. Verapamil in acute myocardial infarction. Br J Clin Pharmacol 1986;21:197S-204S.
DAVIT-II Study. Danish Study Group on Verapamil in Myocardial Infarction. The effects of verapamil on mortal ity and major events after myocardial infarction (the Dan-ish Verapamil Infarction Trial-II). Am J Cardiol 1990;66: 779-785.
ISIS-1 Study. Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction. Lancet 1986;2:56-77.
Ambrosioni E, Borghi C, Magnini B, for the SMILE Study Investiators. The effect of angiotensin converting enzyme inhibitor zofenopril on mortality and morbidity after ante rior myocardial infarction. N Eng J Med 1995;332:80-85.
AIRE Study. The effect of ramipril on mortality andmorbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 1993;342:821-828.
Katz AM. Physiology of the Heart. New York: Raven Press, 1977:324.
Lubbe WF, Podzuweit T, Daries PS, Opie LH. The role of cyclic adenosine monophosphate in adrenergic effects on ventricular vulnerability to fibrillation in the isolated perfused rat heart. J Clin Invest 1978;61:1260-1269.
Verrier RL, Brooks WW, Lown B. Protective zone and the determination of vulnerability to ventricular fibrillation. Am J Physiol 1978;234:H592-596.
Lubbe WF, Peisach M, Pretorius R, Bruyneel KJJ, Opie LH. Distribution of myocardial blood flow before and after coronary artery ligation in the baboon. Relation to early ventricular fibrillation. Cardiovasc Res 1974;8:478-487.
Hearse DJ, Muller CA, Fukanami M, Kudoh Y, Opie LH, Yellon DM. Regional myocardial ischaemia: Characterisation of temporal, transmural and lateral flow interfaces in the porcine heart. Can J Cardiol 1986;2:48-61.
Roberts R, Husain A, Ambos HD, Oliver GC, Cox JR. Sobel BE. Relationship between infarct size and ventricular arrhythmias. Br Heart J 1975;37:1169-1175.
Kaplinsky E, Horowitz A, Neufeld HB. Ventricular reentry and automaticity in myocardial infarction. Effect of size of injury. Chest 1978;74:67-71.
Saveedra JM, Fernandez-Pardal J, Chevillard C. Angiotensin-converting enzyme in discrete areas of the rat forebrain and pituatary gland. Brain Res 1982;245:317-325.
Muller CA, Opie LH, Peisach M, Pineda C. Chronic oral pretreatment by angiotensin converting enzyme inhibitor trandolapril decreases ventricular fibrillation in acute ischemia and reperfusion. Eur Heart J 1994;15:988-996.
Wallenstein S, Zucker CL, Fleiss JL. Some statistical methods useful in circulation research. Circ Res 1980;47:1-9.
Muller CA, Thandroyen FT, Hamm CW, et al. Verapamil and tiapamil in prevention of ventricular fibrillation in pigs with coronary artery ligation. Comparative effects on left ventricular function. Circulation 1988;78:227-232.
Muller CA, Opie LH, McCarthy J, Hofmann D, Pineda CA, Peisach M. Effects of mibefradil, a novel calcium channel blocking agent with T-type activity, in acute experimental myocardial ischemia. J Am Coll Cardiol 1998;32:268-274.
Opie LH, Coetzee WA, Dennis SC, Thandroyen FT. A potential role of calcium ions in early ischemic and reperfusion arrhythmias. Ann NY Acad Sci 1988;522:464-477
Clusin WT, Bristow MR, Karagueuzian HS, Katzung B, Schroeder JS. Do calcium-dependent ionic currents mediate ischemic ventricular fibrillation? Am J Cardiol 1982; 49:606-612.
Kihara Y, Morgan JP. Intracellular calcium and ventricular fibrillation: Studies in the aequorin-loaded isovolumic ferret heart. Circ Res 1991;68:1378-1389.
Coker SJ, McGrath MT. Can captopril modify experimentally induced cardiac arrhythmias? J Mol Cell Cardiol 1985; 17(Suppl. 3):P41.
Rochette L, Ribuot C, Belichard P, Bril A, Devissaguet M. Protective effect of angiotensin converting enzyme inhibitors (CEI) captopril and perindopril on vulnerability to ventricular fibrillation during myocardial ischemia and reperfusion in rat. Clin Exp Hyperten 1987;9:365-368.
Ribuot C, Rochette L. Converting enzyme inhibitors (captopril, enelapril, perindopril) prevent early post infarction ventricular fibrillation in the anaesthetised rat. Cardiovasc Drugs Ther 1987;1:51-55.
De Graeff PA, De Langen CDJ, Van Gilst WH, et al. Protective effect of captopril against ischemia/reperfusion-induced ventricular arrhythmias in vitro and in vivo. Am J Med 1988;84(Suppl. 3A):67-74.
Muller CA, Opie LH, Peisach M, Pineda C. Antiarrhythmic effects of the angiotensin converting enzyme inhibitor perindoprilat in a pig model of acute regional myocardial ischemia. J Cardiovasc Pharmacol 1992;19:748-752.
De Graeff PA, Van Gilst WH, Bel K, De Langen CDJ, Kingma JH, Wesseling H. Concentration-dependent protection by captopril against myocardial damage during ischemia and reperfusion in a closed-chest pig model. J Cardiovasc Pharmacol 1987;9(Suppl. 2):S37-S42.
Tio RA, De Langen DJ, De Graeff PA, et al. The effects of oral pretreatment with zofenopril, an angiotensin II converting enzyme inhibitor, on early reperfusion and subsequent electrophysiologic stability in the pig. Cardiovasc Drug Ther 1990;4:695-704.
Dargie HJ, McAlpine HM, Morton JJ. Neuroendocrine activation in acute myocardial infarction. J Cardiovasc Pharmacol 1987;9(Suppl. 2):S21-24.
Kass RS, Blair ML. Effects of angiotensin II on membrane current in cardiac Purkinje fibres. J Mol Cell Cardiol 1981;13:797-809.
Starke K, Werner U, Hellerforth R, Schumann HJ. Influence of peptides on the output of noradrenaline from isolated rabbit hearts. Eur J Pharmacol 1970;9:136-140.
Schumann HJ, Starke K, Werner U. Interaction of inhibitors of noradrenaline uptake and angiotensin on the sympathetic nerves of the isolated rabbit heart. Br J Pharmacol 1970;39:390-397.
Westfall TC. Local regulation of adrenergic neurotransmission. Physiol Rev 1977;57:659-728.
Roth RH. Action of angiotensin on adrenergic nerve endings: Enhancement of norepinephrine biosynthesis. Fed Proc 1972;31:1358-1364.
Blumberg AL, Ackerly JA, Peach MJ. Differentiation of neurogenic and myocardial angiotensin II receptors in isolated rabbit atria. Circ Res 1975;36:719-726.
Lanier SM, Malik KU. Facilitation of adrenergic transmission in the canine heart by intracoronary infusion of angiotensin II: Effects of prostaglandin synthesis inhibition. J Pharmacol Exp Ther 1983;227:676-682.
Lubbe WF, Podzuweit T, Opie LH. Potential arrhythmogenic role of cyclic AMP and cytosolic calcium overload: Implications for prophylactic effect of beta-blockers in myocardial infarction and proarrhythmic effects of phosphodiesterase inhibitors. J Am Coll Cardiol 1992;19:1622-1633.
Schwieler JH, Hjemdahl P. Influence of angiotensin enzyme inhibition on sympathetic neurotransmission: Possible roles for bradykinin and prostaglandins. J Cardiovasc Pharmacol 1992;(Suppl. 9):S39-S46.
Vegh A, Szekeres L, Parratt JR. Local intracoronary infusions of bradykinin profoundly reduce the severity of ischaemia-induced arrhythmias in anaesthetized dogs. Br J Pharmacol 1991;104:294-295.
Enous R, Coetzee WA, Opie LH. Effect of the ACE inhibitor perindoprilat and of angiotensin II on the transient inward current of guinea pig ventricular myocytes. J Cardiovasc Pharmacol 1992;19:17-23.
Opie LH, Coetzee WA. Role of calcium ions in reperfusion arrhythmias: Relevance to pharmacological intervention. Cardiovasc Drugs Ther 1988;2:623-636.
Linz W, Scholkens BA, Han Y-F. Beneficial effects of the converting enzyme inhibitor ramipril in ischemic rat hearts. J Cardiovasc Pharmacol 1986;8(Suppl. 10):1-30.
Elfellah MS, Ogilvie RI. Effect of vasodilatory drugs on coronary occlusion and reperfusion arrhythmias in anesthetized dogs. J Cardiovasc Pharmacol 1985;7:826-832.
Van Gilst WH, de Graeff PA, Wesseling H, et al. Reduction of reperfusion arrhythmias in the ischemic isolated rat heart by angiotensin converting enzyme inhibitors: A comparison of captopril, enalapril, and HOE 498. J Cardiovasc Pharmacol 1986;8:722-728.
Desta B, Nakashima M, Kirchengast M, Vanhoutte PM, Boulanger CM. Previous exposure to bradykinin unmasks an endothelium-dependent relaxation to the converting enzyme inhibitor trandolaprilat in isolated canine coronary arteries. J Pharmacol Exp Ther 1995;272:885-891.
Kirchengast M, Münter K, Rübsamen K. The CA2+ antagonist verapamil potentiates the effect of the angiotensin-converting enzyme inhibitor trandolapril on cyclic blood flow reductions. J Vasc Med Biol 1994;5:144-151.
Daly P, Mettauer B, Rouleau J-L, Cousineau D, Burgess JH. Lack of reflex increase in myocardial sympathetic tone after captopril: Potential antianginal effect. Circulation 1985;71: 317-25.
Gasic S, Dudczak R, Korn A, Kleinbloesem C. Angiotensin converting enzyme inhibition with cilizapril improves myocardial perfusion to the ischemia regions during exercise: A pilot study. J Cardiovasc Pharmacol 1990;15:227-32
Fischer Hansen J, Hagerup L, Sigurd B, et al. Cardiac event rates after acute myocardial infarction in patients treated with verapamil and trandolapril versus verapamil alone. Am J Cardiol 1997;79:738-741.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Muller, C.A., Opie, L.H., Pineda, C.A. et al. Combination of a Calcium Antagonist, Verapamil, with an Angiotensin Converting Enzyme Inhibitor, Trandolapril, in Experimental Myocardial Ischemia and Reperfusion: Antiarrhythmic and Hemodynamic Effects of Chronic Oral Pretreatment. Cardiovasc Drugs Ther 12, 449–455 (1998). https://doi.org/10.1023/A:1007797931302
Issue Date:
DOI: https://doi.org/10.1023/A:1007797931302