Summary
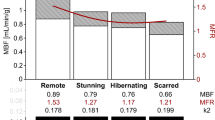
The term hibernating myocardium describes a particular outcome of myocardial ischemia in which myocytes show a chronically depressed contractile ability but remain viable. Revascularization of hibernating tissue causes a recovery of mechanical function that correlates with long-term survival. Therefore it is important clinically to distinguish hibernating from infarcted myocardium, since asynergies due to hibernation will improve on reperfusion, whilst those due to infarct will not. One suggested technique to identify hibernating myocardium is to stimulate the myocytes acutely, but briefly, by administration of inotropic agents while monitoring contractile function by echocardiography. We report our experience on the use of low dosages of dobutamine. Myocardial viability was validated by measuring the recovery in contraction of the akinetic areas after coroanry artery bypass surgery by means of intraoperative epicardial echocardiography. The test has a sensitivity of 93% and a specificity of 78%. It is useful for identification of viable myocardium and also for quantification of intraoperative risk in individual patients. Limitations of this test are related to the presence of downregulation of beta receptors and to the impossibility of differentiating hibernating from stunned myocardium. Another useful technique of identifying hibernating myocardium is the use of radionuclear markers for viability. In our experience the two most important tests are (1) rest-redistribution imaging of thallium 201 (which has a high sensitivity of 93% but a low specificity of 44%) and (2) 99mTe-Sestamibi imaging, which provides information on both perfusion and function with a single injection. This latter technique allows differentiation between stunning and hibernating on the basis of coronary flow, which is preserved in stunning and reduced in hibernation.
Similar content being viewed by others
References
Braunwald E, Kloner RA. The stunned myocardium: Prolonged, postischemic ventricular dysfunction. Circulation 1982;66:1146–1149.
Kloner RA, Ellis SG, Lange R, Braunwald E. Studies of experimental coronary artery reperfusion: Effects of infarct size, myocardial function, biochemistry, ultrastructure, and microvascular damage. Circulation 1983;68(Suppl I):8–15.
Bolli R, Zhu WX, Thornby JI, et al. Time-course and determinants of recovery of function after reversible ischemia in conscious dogs. Am J Physiol 1988;254:H102-H114.
Shen AC, Jennings RB. Kinetics of calcium accumulation in acute myocardial injury. Am J Pathol 1972;67:441–449.
Hearse DJ. Reperfusion of ischaemic myocardium. J Mol Cell Cardiol 1977;9:607–614.
Ferrari R, Raddino R, Di Lisa F, et al. Effects of temperature on myocardial calcium homeostasis and mitochondrial function during ischemia and reperfusion. J Thorac Cardiovasc Surg 1990;99:919–928.
Manning AS, Coltart DJ, Hearse DJ. Ischemia and reperfusion-induced arrhythmias in the rat. Effects of xanthine oxidase inhibition with allopurinol. Circ Res 1984;55: 545–548.
Hearse DJ. Ischemia, reperfusion, and the determinants of tissue injury. Cardiovasc Drugs Ther 1990;4:767–776.
Rahimtoola SH. The hibernating myocardium. Am Heart J 1989;117:211–220.
Rahimtoola SH. A perspective on the three large multiconter randomized clinical trials of coronary bypass surgery for chronic stable angina. Circulation 1985;72(Suppl V):V123-V135.
Braunwald E, Rutherford JD. Reversible ischemic left ventricular dysfunction: Evidence for the “hibernating myocardium.” J Am Coll Cardiol 1986;8:1467–1470.
Rees G, Bristow JD, Kremaku EL, et al. Influence of aortocoronary bypass surgery on left ventricular performance. N Engl J Med 1971;284:116–123.
Chatterjee K, Swan HJC, Parmley WW, et al. Influence of direct revascularization on left ventricular asynergy and function in patients with coronary heart disease. Circulation 1973;47:276–286.
Bonchek LI, Rahimtoola SH, Chaitman BR, et al. Vein graft occlusion: Immediate and late consequences and therapeutic implications. Circulation 1974;50(Suppl II):84–93.
Brundage BH, Massie BM, Botvinick EH. Improved regional ventricular function after successful surgical revascularization. J Am Coll Cardiol 1984;3:902–908.
Rankin JS, Newman GE, Mulhbaier LH, et al. The effect of coronary revascularization on ventricular function in ischemic heart disease. J Thorac Cardiovasc Surg 1985;90: 818–912.
Breisblatt WM, Brown DL, Weiland FL. Reversibility of long-standing left ventricular aneurysm predicted by thallium-201 imaging. J Am Coll Cardiol 1986;7:1162–1120.
Topol EJ, Weiss JL, Guzman PA, et al. Immediate improvement of dysfunctional myocardial segments after coronary revascularization: Detection by intraoperative transesophageal echocardiography. J Am Coll Cardiol 1984;4:1123–1134.
Bodenheimer MM, Banka VS, Hermann GA, et al. Reversible asynergy. Histopathologic and electrographic correlations in patients with coronary artery disease. Circulation 1976;53:792–803.
Cabin HS, Clubb KS, Vita N, Zaret BL. Regional dysfunction by equilibrium radionuclide angiocardiography; a clinicopathological study evaluating the relation of degree of dysfunction to the presence and extent of myocardial infarction. J Am Coll Cardiol 1987;10:743–761.
Tillisch J, Brunken R, Marshal R, et al. Reversibility of cardiac wall motion abnormalities predicted by positron tomography. N Engl J Med 1986;314:884–888.
Carlson EB, Cowley MJ, Wolfgang TC, Vetrovec GW. Acute changes is global and regional rest left ventricular function after successful coronary angioplasty: Comparative results in stable and unstable angina. J Am Coll Cardiol 1989;13:1262–1269.
Cohen M, Charney R, Hershman R, et al. Reversal of chronic ischemic myocardial dysfunction after transluminal coronary angioplasty. J Am Coll Cardiol 1988;12:1193–1204.
Matsuzaki M, Gallagher KP, Kemper WS, et al. Sustained regional dysfunction produced by prolonged coronary stenosis: Gradual recovery after reperfusion. Circulation 1987; 68:170–177.
Fedele FA, Gerwitz H, Capone RJ, et al. Metabolic response to prolonged reduction of myocardial blood flow distal to a severe coronary artery stenosis. Circulation 1988;78:729–736.
Ferrari R, Visioli O. Stunning: Damaging or protective to the myocardium? Cardiovasc Drugs Ther 1991;5:939–946.
Ferrari R, Curello S, Cargnoni A, et al. Metabolic changes during post-ischemic reperfusion. J Mol Cell Cardiol 1988;20:119–133.
Cobbe SM, Poole-Wilson PA. The time of onset and severity of acidosis in myocardial ischaemia. J Mol Cell Cardiol 1980;12:745–749.
Nayler WG, Ferrari R, Poole-Wilson PA, Yepez CE. A protective effect of a mild acidosis an hypoxic heart muscle. J Mol Cell Cardiol 1979;11:1053–1071.
Rahimtoola SH. The stunned and hibernating myocardium (monograph). New York: Am Medica Communications, 1987.
Banka VS, Bodenheimer MM, Helfant RH. Determinants of reversible asynergy: Effect of pathologic Q waves, coronary collaterals, and anatomic location. Circulation 1974; 50:714–719.
Helfant RH, Pine r, Meister SG, et al. Nitroglycerin to unmask reversible asynergy. Correlation with post-coronary bypass ventriculography. Circulation 1974;50:108–113.
Cucchini F, Di Donato M, Ferrari R, Visioli O. Dynamic ventriculography with K-strophanthin. Eur J Cardiol 1978;81:75–84.
Popio KA, Gorlin R, Bechtel D, Levine JA. Postextrasystolic potentiation as a predictor of potential myocardial viability: Preoperative analyses compared with studies after coronary bypass surgery. Am J Cardiol 1977;39:944–953.
Hambly RI, Aintablian A, Wisoff BG, Hartstein ML. Response of the left ventricle in coronary artery disease to postextrasystolic potentiation. Circulation 1975;51:428–435.
Horn HR, Teichholz LE, Cohn PF, et al. Augmentation of left ventricular contraction in coronary artery disease by an inotropic catecholamine. The epinephrine ventriculogram. Circulation 1974;49:1063–1071.
Kimch A, Rozanski A, Fletcher C, et al. Reversal of rest myocardial asynergy during exercise. A radionuclide scintigraphic study. J Am Coll Cardiol 1985;6:1004–1010.
Rozanski A, Berman D, Gray R. Preoperative prediction of reversible myocardial asynergy by postexercise radionuclide ventriculography. N Engl J Med 1982;307:212–216.
Chatterjee K, Swan HJC, Parmley WW, et al. Depression of left ventricular function due to acute myocardial ischemia and its reversal after aortocoronary saphenous-vein bypass. N Engl J Med 1972;286:1117–1122.
Brunken R, Tillisch J, Schwaiger M, et al. Regional perfusion, glucose metabolism, and wall motion in patients with chronic electrocardiographic Q wave infarctions: Evidence for persistence of viable tissue in some infarct regions by positron emission tomography. Circulation 1986;73:951–963.
Schwaiger M. Metabolism and blood flow as new markers of myocardial viability in the evolution of myocardial infarction. Eur J Nucl Med 1986;12:S62-S65.
Goldhaber SZ, Neuvell JB, Alpert NM, et al. Effects of ischaemic like insult on myocardial thallium-201 accumulation. Circulation 1983;67:778–786.
Iskandrian AS, Hakki AH, Kane SA, et al. Rest and redistribution thallium-201 myocardial scintigraphy to predict improvement in left ventricular function after coronary arterial bypass grafting. Am J Cardiol 1983;51:1312–1316.
Tamaki N, Yonekura Y, Yamashita K, et al. Relation of left ventricular perfusion and wall motion with metabolic activity in persistent defects on thallium-201 tomography in healed myocardial infarction. Am J Cardiol 1988;62:202–208.
Fioretti P, Reijs AEM, Neumann D, et al. Improvement in transient and “persistent” perfusion defects on early and late post-exercise thallium-201 tomograms after coronary artery bypass grafting. Eur Heart J 1988;9:1332–1338.
Brunken R, Schwaiger M, McKay MG, et al. Positron emission tomography detects tissue metabolic activity in myocardial segments with persistent thallium perfusion defects. J Am Coll Cardiol 1987;10:557–567.
Kiat H, Berman DS, Maddahl J, et al. Late reversibility of tomographic myocardial thallium-201 defects: An accurate marker of myocardial viability. J Am Coll Cardiol 1988; 12:1456–1463.
Dilsizian V, Rocco TP, Freedman NMT, et al. Enhanced detection of ischemic but viable myocardium by the reinjection of thallium after stress-redistribution imaging. N Engl J Med 1990;323:141–146.
Bonow RO, Dilsizian V, Cuocolo A, Bacharach S. Identification of viable myocardium in patients with chronic coronary artery disease and left ventricular dysfunction. Comparison of thallium scintigraphy with reinjection and PET imaging with 18F-fluorodeoxyglucose. Circulation 1991;83: 26–37.
Freeman I, Grunwald AM, Hoory S, Bodenheimer MM. Effect of coronary occlusion and myocardial viability on myocardial activity of technetium-99m-Sestamibi. J Nucl Med 1991;32:292–298.
Rocco TP, Dilsizian V, Strauss HW, Boucher CA. Technetium-99m isonitrile myocardial uptake at rest. Relation to clinical marker of potential viability. J Am Coll Cardiol 1980;14:1678–1684.
Liu P Technetium-99m-Sestamibi: Another window on myocardial viability? J Nucl Med 1991;32:298–299.
Santoro GM, Bisi G, Sciagara R, et al. Single photon emission computed tomography with technetium-99m hexakis 2-methoxyisobutyl isonitrile in acute myocardial infarction before and after thrombolytic treatment: Assessment of salvaged myocardium and prediction of late functional recovery. J Am Coll Cardiol 1990;15:301–314.
Wackers FJ. Thrombolytic therapy for myocardial infarction: Assessment of efficacy by myocardial perfusion imaging with technetium-99m Sestamibi. Am J Cardiol 1990;66:36E-41E.
Jones RH, Borges-Neto S, Potts JM. Simultaneous measurement of myocardial perfusion and ventricular function during exercise from a single injection of technetium-99m Sestamibi in coronary artery disease. Am J Cardiol 1990; 66:68E-71E.
Becker LC, Levine JH, Di Paula AF, et al. Reversal of dysfunction in postischemic stunned myocardium by epinephrine and postextrasystolic potentiation. J Am Coll Cardiol 1986;7:580–589.
Bolli R, Zhu WX, Myers ML, et al. Beta-adrenergic stimulation reverses postischemic myocardial dysfunction without producing subsequent functional deterioration. Am J Cardiol 1985;56:946–948.
Pierard LA, De Landsheere C, Berthe C, et al. Identification of viable myocardium by echocardiography during dobutamine infusion in patients with myocardial infarction after thrombolytic therapy: Comparison with positron emission tomography. J Am Coll Cardiol 1990;15:1021–1031.
Alderman EL, Fisher LD, Litwin P, et al. Results of coronary artery surgery in patients with poor left ventricular function (CASS). Circulation 1983;68:785–795.
Coles JG, Del Campo C, Ahmed SH, et al. Improved longterm survival following myocardial revascularization in patients with severe left ventricular dysfunction. J Thorac Cardiovasc Surg 1981;81:846–850.
Califf RM, Harrell FE, Lee KL, et al. Changing efficacy of coronary revascularization. Implications for patient selection. Circulation 1988;78(Suppl I):I185-I191.
Mintz LY, Ingels NBJr., Daughters GI, et al. Sequential studies of left ventricular function and wall motion after coronary bypass surgery. Am J Cardiol 1980;45:210–216.
Topol EJ, Weiss JL, Guzman PA, et al. Immediate improvement of dysfunctional myocardial segments after coronary revascularization: Detection by intraoperative transesophageal echocardiography. J Am Cardiol 1984;4:1123–1134.
Lazar HL, Plehn JF, Schick EM, et al. Effects of coronary revascularization on regional wall motion. An intraoperative two-dimensional echocardiographic study. J Thorac Cardiovasc Surg 1989;98:498–505.
Bashour TT, Mason D. Myocardial hibernation and “embalment.” Am Heart J 1990;119:706–708.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ferrari, R., La Canna, G., Giubbini, R. et al. Hibernating myocardium in patients with coronary artery disease: Identification and clinical importance. Cardiovasc Drug Ther 6, 287–293 (1992). https://doi.org/10.1007/BF00051152
Issue Date:
DOI: https://doi.org/10.1007/BF00051152