Abstract
Objectives
Noncardiac findings are common on coronary computed tomography angiography (CCTA). We assessed the clinical impact of noncardiac findings, and potential changes to surveillance scans with the application of new lung nodule guidelines.
Methods
This substudy of the SCOT-HEART randomized controlled trial assessed noncardiac findings identified on CCTA. Clinically significant noncardiac findings were those causing symptoms or requiring further investigation, follow-up or treatment. Lung nodule follow-up was undertaken following the 2005 Fleischner guidelines. The potential impact of the 2015 British Thoracic Society (BTS) and the 2017 Fleischner guidelines was assessed.
Results
CCTA was performed in 1,778 patients and noncardiac findings were identified in 677 (38%). In 173 patients (10%) the abnormal findings were clinically significant and in 55 patients (3%) the findings were the cause of symptoms. Follow-up imaging was recommended in 136 patients (7.6%) and additional clinic consultations were organized in 46 patients (2.6%). Malignancy was diagnosed in 7 patients (0.4%). Application of the new lung nodule guidelines would have reduced the number of patients undergoing a follow-up CT scan: 68 fewer with the 2015 BTS guidelines and 78 fewer with the 2017 Fleischner guidelines; none of these patients subsequently developed malignancy.
Conclusions
Clinically significant noncardiac findings are identified in 10% of patients undergoing CCTA. Application of new lung nodule guidelines will reduce the cost of surveillance, without the risk of missing malignancy.
Key Points
• Clinically significant noncardiac findings occur in 10% of patients undergoing CCTA.
• Noncardiac findings may be an important treatable cause of chest pain
• Further imaging investigations for noncardiac findings were recommended in 8% of patients after CCTA.
• New lung nodule follow-up guidelines will result in cost savings.
Similar content being viewed by others
Introduction
The SCOT-HEART prospective multicentre randomized controlled trial showed that coronary computed tomography angiography (CCTA) in patients with suspected angina due to coronary heart disease improves diagnostic certainty, changes management and reduces future rates of myocardial infarction. [9] This has led to important changes in national guidelines which recommend the increased use of CCTA in patients with stable chest pain [1]. However, CCTA images visualize more than just the heart, and noncardiac findings can be an important cause of symptoms or require further investigation and management. With the increased use of CCTA, it is important to understand the downstream consequences of such noncardiac findings.
The follow-up of incidental lung nodules identified on computed tomography (CT) is dependent on local, national and international guidelines. In the SCOT-HEART trial, the 2005 Fleischner Society guidelines [2] were used to provide recommendations regarding lung nodule follow-up. These have recently been superseded by the 2015 British Thoracic Society (BTS) guidelines [3] and the 2017 Fleischner Society guidelines [4]. Trials of CT screening in patients at high risk of lung cancer have also established that CT of the chest can identify early lung cancers and reduce mortality in a cost-effective manner [5,5,7]. CCTA is often performed in patients with risk factors similar to those screened for lung cancer, such as smokers over the age of 55 years. Therefore, it is important to identify lung nodules on CCTA which may require further investigation and management.
In this substudy of the SCOT-HEART trial, we assessed the frequency and follow-up of noncardiac findings. In addition, we assessed the impact of changes in lung nodule follow-up guidelines on downstream investigations and costs.
Materials and methods
Study design and participants
The SCOT-HEART study was a multicentre randomized control trial of the use of CCTA in outpatients with suspected angina due to coronary artery disease [8]. The primary results of the SCOT-HEART study have been published [9]. Briefly, 4,146 patients who attended the Cardiology Outpatient Clinic were randomized to standard care or CT plus standard care, and followed up for symptoms, management and outcomes. Of these, 2,073 patients were randomized to CCTA, of whom 1,778 underwent CCTA. CCTA and non-contrast imaging for calcium scoring were performed as described previously [9], and this included a full field of view reconstruction of the chest in addition to CCTA reconstructions.
Assessment of noncardiac findings
The presence of noncardiac findings was assessed on CCTA images focused on the heart, and also on the wide field of view images reconstructed to cover the entire scanned volume. In patients with partially imaged noncardiac findings identified at the time of scanning, a further full thoracic scan was not immediately performed, but could be subsequently recommended by the reporting radiologist. Images were reconstructed with standard soft tissue and lung reconstruction algorithms from each scanner. The reporting radiologist used soft tissue, lung and bone windowing parameters to view the images, with further manual adjustment as required.
Noncardiac findings were recorded by the reporting radiologist and the results were provided to the clinical team along with the CCTA results. Whether noncardiac findings were the cause of the patient’s symptoms was assessed on a four-point scale (‘yes’, ‘probable’, ‘unlikely’ or ‘no’). Clinically significant noncardiac findings were defined as those causing symptoms (‘yes’ or ‘probable’) or incidental findings requiring further investigation, follow-up or treatment.
Assessment of lung nodules
Recommendations for lung nodule follow-up were provided to clinicians according to the 2005 Fleischner Society guidelines [2]. We assessed the potential change to the management of lung nodules if the 2015 BTS guidelines [3] and the 2017 Fleischner Society guidelines had been applied [4]. The lungs were assessed on wide field of view images reconstructed using a standard lung reconstruction algorithm. Lung nodule diameter was measured as the maximum diameter in any transverse projection, rounded to the nearest millimetre. Lung nodule volume was determined using Carestream Vue PACS (version 11; Carestream Health, Rochester, NY).
Follow-up of noncardiac findings
Information on subsequent investigations for noncardiac findings were obtained from electronic health records. Information on clinic consultations were obtained from electronic health records or paper records where required. Imaging costs were obtained from the NHS Reference costs for 2014-2015 (Table 4) [10].
Statistical analysis
Statistical analysis was performed using SPSS (version 23 for Mac OS X; IBM Corp., Armonk, NY). Normally distributed quantitative variables are presented as means and standard deviations. Non-normally distributed data are presented as medians and interquartile ranges (IQR). Statistical significance was assessed using Student’s t test, the Mann-Whitney U test or the chi-squared test as appropriate, and relative risks (RR) were calculated. A statistically significant difference was defined as a two-sided p value of <0.05.
Results
Noncardiac findings
Of the 1,778 patients who underwent CCTA, noncardiac findings were reported in 675 (38%). Patients with noncardiac findings were slightly older (60 ± 9 vs. 56 ± 9 years; p < 0.001) but there were no differences in gender, body mass index or presence of diabetes mellitus (Table 1). Patients who were current smokers or ex-smokers were more likely to have noncardiac findings than nonsmokers (RR 1.38, 95% confidence interval, CI, 1.22–1.56; p < 0.001). Patients with moderate or obstructive coronary artery disease were slightly more likely to have noncardiac findings than patients with mild disease or normal coronary arteries (RR 1.18, 95% CI 1.05–1.34; p = 0.005).
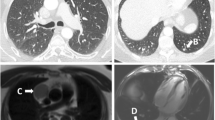
In 175 of the 675 patients with noncardiac findings, the findings were defined as clinically significant (10% of all those undergoing CCTA, and 26% of those with noncardiac findings). There were no differences in age, gender, body mass index, presence of diabetes mellitus or presence of obstructive coronary artery disease between those with significant and those with nonsignificant noncardiac findings. The commonest findings were lung nodules or masses, emphysema and hiatus hernia (Table 2, Fig. 1). Noncardiac findings were deemed to be the definite cause of symptoms in 22 patients (1.2% of those undergoing CCTA, and 3.3% of those with noncardiac findings), and the probable cause of symptoms in a further 33 patients (1.9% and 4.9%, respectively). This included five patients (0.3% of those undergoing CCTA) with pulmonary emboli (Fig. 2).
Investigation and management of noncardiac findings
Further imaging investigations for noncardiac findings were performed in 136 patients (7.6% of those undergoing CCTA, 20% of those with noncardiac findings). The most frequent follow-up imaging was CT for lung nodule assessment followed by ultrasonography of the liver and CT follow-up of other noncardiac findings (Table 3). Smokers were slightly more likely to undergo follow-up imaging (RR 1.41, 95% CI 1.02–1.96; p = 0.04), but there were no differences in rates of follow-up in relation to age, body-mass index, presence of diabetes mellitus or presence of obstructive coronary artery disease.
Additional clinic consultations were organized in 46 patients (2.6% of those undergoing CCTA, 7% of those with noncardiac findings). The most frequent specialty to which patients were referred was the respiratory clinic (Table 3). There were no differences between patients who did or did not have follow-up in terms of age, body mass index, presence of diabetes mellitus, smoking status or presence of obstructive coronary artery disease.
Patients with respiratory infection, pulmonary embolism and malignancy identified on CCTA received appropriate therapy. In two patients with malignancy, the disease was too advanced at presentation and palliative management was given. The remaining patients underwent surgery (one patient), chemotherapy (one), chemotherapy and radiotherapy (one), pleurodesis (one), and chemoembolization (one). In contrast, there was no increase in gastric acid suppressant medication (RR 0.84, 95% CI 0.53–1.34; p = 0.466) in patients with a hiatus hernia nor were there demonstrable changes to treatment in patients with emphysema.
Outcomes of patients with non-cardiac findings
Malignancy was diagnosed in seven patients who underwent investigation for noncardiac findings (0.4% of patients undergoing CCTA, 3.5% of those with lung nodules). Malignancies included lung cancer (four patients) (Fig. 3), mesothelioma (one), metastatic testicular cancer (one) and hepatocellular carcinoma (one; Fig. 2). In patients with clinically significant noncardiac findings, there was no statistically significant difference in all-cause mortality (RR 2.50, 95% CI 0.70–8.87; p = 0.157).
Lung nodules
Lung nodules, masses or granuloma were identified on CCTA in 200 patients (11% of those undergoing CCTA): ≤4 mm in 119 (60%), 5–7 mm in 58 (29%) and ≥8 mm in 23 (12%). Lung nodules were more common in current smokers or ex-smokers (RR 1.58, 95% CI 1.20–2.08; p = 0.001) but were not associated with age, gender, or presence of obstructive coronary artery disease. In 118 (59%) of the patients with lung nodules, semiautomated measurement of nodule volume was possible. The median lung nodule volume was 55 mm3 (IQR 32–116 mm3). Volume measurements were not possible in the remaining patients due to the small size of the lesions, proximity to structures of similar density, such as the pleura or diaphragm, or technical reasons.
Follow-up imaging for lung nodule assessment was recommended in 126 patients (7% of those undergoing CCTA). One patient died before follow-up imaging could be performed and 40 patients (20% of those with lung nodules) did not undergo follow-up imaging due to physician or patient choice. Thus 85 patients (4.7% of those undergoing CCTA) underwent CT follow-up for lung nodules. The median follow-up duration was 12 months (IQR 7–19 months) and the median number of CT scans performed was 1 (IQR 1–2). The first follow-up CT scan was performed at a median of 7 months after the initial CCTA scan (IQR 3.5–9.0 months), the second at 14 months (IQR 10.3–20.8 months), the third at 24 months (IQR 15–25.5 months) and the fifth at 31 months (IQR 26.8–35.3 months).
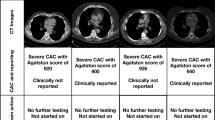
Application of new lung nodule guidelines
The 2015 BTS guidelines suggest that no follow-up is required for lung nodules <5 mm or <80 mm3. In the SCOT-HEART study, this means that 68 fewer scans would have been performed in 47 patients, all of whom were subsequently discharged from follow-up without evidence of malignancy. This would have reduced the number of patients with significant lung nodules requiring follow-up to 38 (2% of patients undergoing CCTA). The 2017 Fleischner Society guidelines suggest that no follow-up is required for lung nodules of <6 mm or <100 mm3. In the SCOT-HEART study this means that 78 fewer scans would have been performed in 53 patients, all of whom were subsequently discharged from follow-up without evidence of malignancy. This would have reduced the number of patients with significant lung nodules requiring follow-up to 32 (2% of patients undergoing CCTA).
The cost of follow-up imaging for noncardiac findings was £10.06 per patient undergoing CCTA (1,778 patients, Table 4). The cost of imaging for lung nodule follow-up was £147.25 per patient undergoing lung nodule follow-up (85 patients) and £7.04 per patient undergoing CCTA (1,778 patients, Table 5). Applying the 2015 BTS guidelines would have reduced the cost per patient undergoing CCTA to £3.52 and applying the 2017 Fleischner Society guidelines would have reduced the cost to £3.00. This equates to 50% and 57% reductions in cost, respectively (Table 5).
Discussion
Although noncardiac findings on CCTA are common, only one quarter of these are clinically significant. Occasionally, these findings identify an important treatable cause of the patient’s chest pain but usually they represent important incidental findings that require surveillance, especially lung nodules. The application of new guidelines for lung nodule assessment will reduce the number of follow-up CT scans required in these patients, without the risk of missing malignancy identified during screening, and will significantly reduce the cost of follow-up imaging.
Frequency and implications of noncardiac findings
The frequency of noncardiac findings in patients undergoing CCTA varies widely, and depends on the classification of findings and the population profile, such as age and frequency of smoking habit. A systematic review identified an average prevalence of 41% for noncardiac findings and 16% for clinically significant findings [11]. Our rates of noncardiac findings and significant findings were similar but slightly lower at 38% and 10%, respectively. This was possibly due to the wide inclusion criteria of the SCOT-HEART study, and the focus on a narrow detector range reducing both radiation dose and the scanned body volume.
Causes of chest pain can be challenging to diagnose. Patients in the SCOT-HEART trial were referred because of concern that they had angina pectoris due to coronary heart disease. In the CCTA group, ultimately 696 patients (33%) were diagnosed with this condition. In contrast, only a further 55 patients (3%) were diagnosed with alternative conditions that accounted for their symptoms including pneumonia, pulmonary embolism and cancer. This suggests a very modest rate of noncardiac causes of chest pain in this population. However, some of these noncardiac causes of chest pain are serious and potentially life-threatening, underlining the importance of full and comprehensive scan reporting including noncardiac structures.
Lung nodule follow-up
The lungs were the commonest location of noncardiac findings in the SCOT-HEART study. This is similar to the findings of previous studies [11] and was largely driven by the prevalence of emphysema and lung nodules. The link between cardiovascular disease and respiratory diseases, such as emphysema, is complex and includes shared risk factors such as smoking and chronic inflammation [12, 13]. Lung cancer is the most frequent cause of death from cancer worldwide [5]. The National Lung Screening Trial (NLST) recruited asymptomatic participants aged 55 to 74 years, with a 30 pack-year smoking history and who were current smokers or had stopped smoking in the previous 15 years. The NLST identified a 20% (95% CI 6.8–26.7; p = 0.004) relative reduction in lung cancer mortality among 26,722 patients undergoing low-dose CT screening as compared with 26,732 patients undergoing plain radiography chest screening [14].
The NELSON study recruited 15,822 patients aged 50 to 75 years, who had smoked ≥15 cigarettes per day for ≥25 years or ≥10 cigarettes per day for ≥30 years and who were current smokers or had ceased smoking in the previous 10 years [15]. Participants were randomized 1:1 to CT screening or standard care. Early reports identified a beneficial effect of a screening interval of 2 years compared with 2.5 years [6], but at the time of this report the full trial results were awaited. The UK Lung Cancer Screening (UKLS) trial recruited 249,988 participants aged 50 to 75 years who had a ≥5% 5-year lung cancer risk based on the Liverpool Lung Project version 2 risk prediction model [7]. Participants were randomized 1:1 to CT screening or standard care. Pilot results showed that lung cancer could be identified at an early stage with potentially curative treatment possible in over 80% of patients [7]. However, at the time of this report the full results were also awaited.
The US Preventive Services Task Force recommends annual CT lung cancer screening in people aged 55 to 80 years, with a 30 pack-year history, and who were current smokers or had stopped smoking within the past 15 years [16]. The proportion of patients with lung nodules in the SCOT-HEART study was lower than in the lung cancer screening trials. This is probably partly due to the lower risk in the SCOT-HEART population, which included younger patients and nonsmokers. In addition, only part of the lungs are imaged on the wide field of view reconstruction from CCTA images as the scan range is selected to cover just the length of the heart rather than the full thorax. CCTA therefore does not image the upper parts of the lungs, a frequent location for lung cancer [17].
New lung nodule follow-up guidelines
The new revised lung nodule follow-up guidelines have changed the threshold for lung nodules that require follow-up. In the 2015 BTS guidelines, no follow-up is required for “clearly benign lesions”, lesions <5 mm maximum diameter or lesions <80 mm3 volume [3]. In the 2017 Fleischner guidelines, no follow-up is required for single nodules <6 mm average diameter or <100 mm3 volume, but nodules with “suspicious” morphology or located in the upper lobe may be considered for a follow-up scan at 12 months [4]. Both new guidelines include the assessment of lung nodule volume rather than diameter as a potentially more reproducible method of assessment [4]. However, the value of automated lung nodule volume measurement is limited as only 59% of patients with lung nodules could be assessed in our study. In addition, whether maximum or average diameter is used may also affect the results. We retrospectively applied these diameter and volume criteria to the SCOT-HEART data which means we may have underestimated the benefit of the 2015 BTS guidelines and overestimated the benefit of the 2017 Fleischer guidelines. Nevertheless, we have shown that the application of these guidelines would lead to significant cost savings.
Previous studies have shown that the direct cost of imaging for significant incidental findings are between US$438 and US$606 [11, 18, 19]. The cost of follow-up imaging for significant noncardiac findings was lower in the SCOT-HEART study than in previous studies with a cost per patient of £10.06 averaged across all patients undergoing CCTA. However, there were significant differences in the healthcare systems involved in previous studies and therefore these figures are not directly comparable. There may also have been differences in the classification of significant noncardiac findings, in –the estimation of costs and in follow-up guidelines. In addition, the total cost of follow-up in the SCOT-HEART study should also include downstream clinic attendances and other nonimaging investigations which were not included in this estimate. The use of the national picture archiving system (PACS), that has been available in Scotland since 2008, for follow-up imaging means that any imaging performed in Scotland can be identified. However, a small number of patients may be missing if they have moved out of Scotland.
It is interesting to note that 20% of patients in whom subsequent imaging for lung nodule assessment was recommended did not undergo further imaging. This is a limitation of this study, but does highlight the real-world implications of the identification of noncardiac findings on CCTA. A variety of factors have been found to influence referral for further imaging including patient and physician factors [20].
Conclusions
Significant noncardiac findings occur in 10% of patients undergoing CCTA for suspected angina due to coronary heart disease. Occasionally, these findings identify an important treatable cause of the patient’s chest pain but usually they represent important incidental findings that require surveillance, especially lung nodules. The application of new guidelines for lung nodule assessment will reduce the number of follow-up CT scans required in these patients, without the risk of missing malignancy identified during screening, and will significantly reduce the cost of follow-up imaging.
References
NICE (2016) Chest pain of recent onset: assessment and diagnosis. National Institute for Health and Care Excellence, London
MacMahon H, Austin JHM, Gamsu G, Herold CJ, Jett JR, Naidich DP, Patz EF, Swensen SJ (2005) Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 237(2):395–400
Callister MEJ, Baldwin DR, Akram AR et al (2015) British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 70:ii1–ii54
MacMahon H, Naidich DP, Goo JM et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology 284:228–243
National Lung Screening Trial Research Team, Church TR, Black WC et al (2013) Results of initial low-dose computed tomographic screening for lung cancer. N Engl J Med 368:1980–1991
Yousaf-Khan U, van der Aalst C, de Jong PA et al (2017) Final screening round of the NELSON lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax 72:48–56
Field JK, Duffy SW, Baldwin DR et al (2016) UK Lung Cancer RCT Pilot Screening Trial: baseline findings from the screening arm provide evidence for the potential implementation of lung cancer screening. Thorax 71:161–170
Newby DE, Williams MC, Flapan AD et al (2012) Role of multidetector computed tomography in the diagnosis and management of patients attending the rapid access chest pain clinic, The Scottish computed tomography of the heart (SCOT-HEART) trial: study protocol for randomized controlled trial. Trials 13:184
SCOT-HEART investigators (2015) CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 385:2383–2391
Department of Health. NHS Reference costs 2014-2015. November 2015. Accessed via https://www.gov.uk/government/publications/nhs-reference-costs-2014-to-2015 on 14 May 2017.
Karius P, Schuetz GM, Schlattmann P, Dewey M (2014) Extracardiac findings on coronary CT angiography: a systematic review. J Cardiovasc Comput Tomogr 8:174–182.e6
Williams MC, Murchison JT, Edwards LD et al (2014) Coronary artery calcification is increased in patients with COPD and associated with increased morbidity and mortality. Thorax 69:718–723
Chen W, Thomas J, Sadatsafavi M, FitzGerald JM (2015) Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med 3:631–639
National Lung Screening Trial Research Team, Aberle DR, Adams AM et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409
van Iersel CA, de Koning HJ, Draisma G, Mali WPTM, Scholten ET, Nackaerts K, Prokop M, Habbema JDF, Oudkerk M, van Klaveren RJ (2007) Risk-based selection from the general population in a screening trial: selection criteria, recruitment and power for the Dutch-Belgian randomised lung cancer multi-slice CT screening trial (NELSON). Int J Cancer 120:868–874
Moyer VA, U.S. Preventive Services Task Force (2014) Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 160:330–338
McWilliams A, Tammemägi MC, Mayo JR et al (2013) Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med 369:910–919
Lee CI, Tsai EB, Sigal BM, Plevritis SK, Garber AM, Rubin GD (2010) Incidental extracardiac findings at coronary CT: clinical and economic impact. AJR Am J Roentgenol 194:1531–1538
Bendix K, Jensen JM, Poulsen S, Mygind N, Nørgaard BL (2011) Coronary dual source multi detector computed tomography in patients suspected of coronary artery disease: prevalence of incidental extra-cardiac findings. Eur J Radiol 80:109–114
Young B, Bedford L, Kendrick D, Vedhara K, Robertson JFR, das Nair R (2017) Factors influencing the decision to attend screening for cancer in the UK: a meta-ethnography of qualitative research. J Public Health (Oxf):1–25. https://doi.org/10.1093/pubmed/fdx026
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Professor David Newby.
Conflict of interest
The authors of this manuscript declare relationships with the following companies. D.E.N., E.J.R.v.B., and G.R. have received honoraria and consultancy from Toshiba Medical Systems. G.R. has received honoraria from companies producing contrast media (Bracco, Bayer-Schering, GE Healthcare and Guerbet). M.C.W. has performed consultancy from GE Healthcare.
Funding
This study received funding from the Chief Scientist Office of the Scottish Government Health and Social Care Directorates (CZH/4/588), with supplementary awards from Edinburgh and Lothian’s Health Foundation Trust and the Heart Diseases Research Fund. D.E.N. (CH/09/002) and M.C.W. (FS/11/014) are supported by the British Heart Foundation. D.E.N. is the recipient of a Wellcome Trust Senior Investigator Award (WT103782AIA). E.J.R.v.B. is supported by the Scottish Imaging Network: A Platform for Scientific Excellence (SINAPSE). The Royal Bank of Scotland supported the provision of 320-multidetector CT for NHS Lothian and the University of Edinburgh. The Edinburgh Imaging facility QMRI (Edinburgh) is supported by National Health Service Research Scotland (NRS) through the National Health Service Lothian Health Board. The Clinical Research Facility Glasgow and Clinical Research Facility Tayside are supported by NRS. M.C.W is supported by The Chief Scientist Office of the Scottish Government Health (PCL/17/04).
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported with the primary results of the SCOT-HEART study published in the Lancet (https://www.ncbi.nlm.nih.gov/pubmed/25788230). However, there is no significant overlap with this paper.
Methodology
• retrospective
• controlled trial
• multicentre study
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Williams, M.C., Hunter, A., Shah, A.S.V. et al. Impact of noncardiac findings in patients undergoing CT coronary angiography: a substudy of the Scottish computed tomography of the heart (SCOT-HEART) trial. Eur Radiol 28, 2639–2646 (2018). https://doi.org/10.1007/s00330-017-5181-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5181-5