Abstract
Background
Renal denervation (RDN) may lower blood pressure (BP); however, it is unclear whether medication changes may be confounding results. Furthermore, limited data exist on pattern of ambulatory blood pressure (ABP) response—particularly in those prescribed aldosterone antagonists at the time of RDN.
Methods
We examined all patients treated with RDN for treatment-resistant hypertension in 18 UK centres.
Results
Results from 253 patients treated with five technologies are shown. Pre-procedural mean office BP (OBP) was 185/102 mmHg (SD 26/19; n = 253) and mean daytime ABP was 170/98 mmHg (SD 22/16; n = 186). Median number of antihypertensive drugs was 5.0: 96 % ACEi/ARB; 86 % thiazide/loop diuretic and 55 % aldosterone antagonist. OBP, available in 90 % at 11 months follow-up, was 163/93 mmHg (reduction of 22/9 mmHg). ABP, available in 70 % at 8.5 months follow-up, was 158/91 mmHg (fall of 12/7 mmHg). Mean drug changes post RDN were: 0.36 drugs added, 0.91 withdrawn. Dose changes appeared neutral. Quartile analysis by starting ABP showed mean reductions in systolic ABP after RDN of: 0.4; 6.5; 14.5 and 22.1 mmHg, respectively (p < 0.001 for trend). Use of aldosterone antagonist did not predict response (p > 0.2).
Conclusion
In 253 patients treated with RDN, office BP fell by 22/9 mmHg. Ambulatory BP fell by 12/7 mmHg, though little response was seen in the lowermost quartile of starting blood pressure. Fall in BP was not explained by medication changes and aldosterone antagonist use did not affect response.
Similar content being viewed by others
Introduction
Hypertension contributes to 62 % of all strokes, 49 % of global heart disease burden and causes an estimated 7.1 million deaths a year [1, 2]. In most real-world datasets, however, fewer than 50 % of subjects are at target despite a range of pharmacological options. The reasons for this are complex, but it seems clear that new strategies for the management of uncontrolled hypertension are required [3, 4].
Reduction of sympathetic outflow is one proposed alternative to drug treatment for reducing high blood pressure. Invasive surgical sympathectomy was shown to lead to significant blood pressure reductions over 70 years ago; however, this procedure was abandoned due a high complication rate [5]. Renal artery sympathetic denervation aims to more selectively abrogate efferent and afferent sympathetic nerve signals to and from the kidney, to reduce sympathetic nervous activity and therefore blood pressure [6, 7].
Early observational data and open-label, randomized studies suggested substantial reductions in blood pressure following a single percutaneous procedure [8, 9]. Reduction in sympathetic tone through RDN also appeared to be associated with potential beneficial effects on hypertension end-organ effects and in other conditions where sympathetic drive may modulate the disease condition [10–16].
More recently, a rigorously conducted randomized trial added renal denervation (RDN) to a stepped anti-hypertensive drug program and demonstrated incremental blood pressure lowering with RDN [17]. However, a sham-controlled trial of RDN (symplicity HTN-3) failed to meet its primary efficacy endpoint [18]. The procedure met its safety endpoint, but similar reductions in blood pressure were seen between the renal denervation group and the sham-control group. Secondary sub-analyses of the trial dataset by the authors have suggested potential confounders, principal amongst them being that fewer than 6 % of patients received per-protocol bilateral retrograde spiral ablation [19].
The efficacy of this technology therefore remains uncertain and further randomized trials are required. In the meantime, more data are required on the nature of the patients who have already undergone the procedure, their response to treatment and identification of factors that may affect subsequent blood pressure response. Such data would better inform the design, conduct and interpretation of future trials.
This article reports the UK experience with RDN for treatment-resistant hypertension. It examines the nature of the blood pressure response seen on ambulatory monitoring and the impact of drug changes post denervation on the results. Finally, this study examines the interaction of RDN with the use of aldosterone antagonists.
Methods
At the time of instigation of the UK Renal Denervation Affiliation (May 2014), background research by the study team identified 21 centers that had performed five or more procedures in the UK. The aim of this study was to give as complete as possible a representation of the UK national experience with RDN to date, by collating retrospective data from all procedures performed on patients with uncontrolled hypertension.
Each center was contacted by email and/or telephone and invited to participate in the registry. Eighteen of those centers agreed to contribute and provided the data that form the basis for this manuscript. These data represent the results of cases performed for treatment-resistant hypertension, as defined by prior international consensus statements [7] and in accordance with the Joint UK Societies consensus statement [20]. A small number of cases were excluded as they were performed for other indications as part of ongoing clinical trials (e.g. heart failure; sleep apnea; acknowledged non-compliance with medications).
Anonymized data were collated locally using a spreadsheet specifically designed for the study and then submitted to a central coordinating center (Exeter, UK), where it was analyzed. The project was independent of any financial support from industry and is an exclusively investigator-led initiative.
‘Responders’ to RDN are defined according to prior convention [21], by a reduction in office systolic blood pressure of ≥10 mmHg and reduction in daytime ambulatory systolic blood pressure fall of ≥5 mmHg from baseline to follow-up [18]. Absence of normal nocturnal dipping profile on pre-procedural ABP was defined as a fall in nighttime systolic ABP of <10 %. The lattermost BP readings available are reported.
Data are presented as mean ± standard deviation (SD) unless stated. Between group variations were analyzed using Chi Square test for categorical variables and where normality was demonstrated, a T test or ANOVA were used for continuous variables. Logistic regression models were used to examine the interaction of aldosterone antagonist use with blood pressure response following RDN after adjustment for factors previously thought to interact with response to RDN from prior literature. These models were also used to look for other potential baseline predictors of blood pressure changes after RDN. A p value of <0.05 was considered statistically significant. Statistical analyses were performed using SPSS software v20.0 (SPSS Inc. Chicago, IL).
Results
Results from 253 subjects, treated in 18 centers using five different technologies, are included in this analysis. These include Symplicity Flex [n = 204 (81 %)]; Symplicity Spyral [n = 10 (4 %)]; Boston Vessix [n = 3 (1 %)]; St Jude Enlightn [n = 26 (10 %)] and Covidien Oneshot [n = 10 (4 %)]. Mean age of patients was 57 years; 53 % were female; 88 % Caucasian and 26.5 % were diabetic (Table 1).
Eighty-six percent of patients were seen in a dedicated hypertension clinic with each patient being reviewed by an average of 1.6 hypertension specialists. These included cardiologists, nephrologists, clinical pharmacologists and endocrinologists. All patients had anatomical screening of their renal arteries prior to their RDN procedure.
The majority of patients had pre-procedural ambulatory blood pressure monitoring performed (73.5 %) and detailed assessments to rule out secondary hypertension before the procedure (screening details are shown in Table 2).
Mean office BP before procedure was 185/102 mmHg (SD 26/19; n = 253) with an average daytime ambulatory blood pressure (ABP) of 170/98 mmHg (SD 22/16; n = 186). Fifty-eight percent of the cohort had loss of normal nocturnal dipping on ABP. The median number of antihypertensive drugs prescribed before RDN was 5.0 including 96 % ACEi/ARB; 86 % thiazide or a loop diuretic and 55 % aldosterone antagonist prescription at the time of denervation (Tables 3, 4).
Clinical follow-up was available in 90 % of subjects, with mean duration of office BP follow-up of 11 months. Mean post-procedural office BP was 163/93 mmHg, representing a fall in office BP following RDN of 22/9 mmHg.
ABP data were available in 70 % of cases post-procedure, at a mean follow-up duration of 8.5 months. Average daytime ABP at the end of follow-up was 158/91 mmHg, representing a fall in daytime ABP following RDN of 12/7 mmHg. Average number of antihypertensive agents added per patient was 0.36. Average number of agents withdrawn per patient was 0.91 (Tables 5, 6). Drug dose changes appeared to be balanced across the cohort, in terms of dose escalation and reductions.
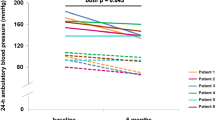
Figure 1 shows BP response to RDN according to quartile of baseline daytime ambulatory systolic BP. Baseline mean daytime ambulatory systolic BP (ASBP) from quartile 1 to 4 was: 142, 162, 176 and 199 mmHg, respectively. Number of antihypertensive drugs per quartile did not significantly differ (p > 0.2). At 8.5 months follow-up, the mean reductions in daytime ASBP by quartile of starting daytime ASBP were: 0.4; 6.5; 14.5 and 22.1 mmHg, respectively (p value for quartile trend <0.001).
Office systolic BP (OSBP) also exhibited significant falls across each of the four quartiles (p = 0.001 for quartile trend), but in the lowest quartile, this was not matched by a statistically significant ASBP response. Overall, 65 % patients were defined as responders, with a ≥10 mmHg fall in OSBP. A similar percentage (62 %) had a ≥5 mmHg fall in daytime ASBP.
Use of aldosterone antagonist at the time of RDN did not predict the degree of blood pressure response (p > 0.2 as univariate predictor). This remained the case after adjustment for the following potential confounders: age, gender, diabetes, estimated glomerular filtration rate (eGFR), number of drugs taken and starting office blood pressure (p > 0.2). There remained no association when ASBP was substituted for OSBP within the model. The only baseline characteristic that predicted subsequent fall in BP after RDN was blood pressure, as measured by office or ABP.
Discussion
This investigator-led study reports the results of RDN procedures for 253 people with treatment-resistant hypertension, performed in 18 UK specialist centers using five different technologies. It shows significant reductions in both office and daytime ambulatory blood pressure of 22/9 and 12/7 mmHg, respectively, after a mean follow-up period of 11 months (p < 0.001 for both findings). This blood pressure reduction does not appear to be related to changes in anti-hypertensive medications made after denervation and use of aldosterone antagonists did not affect blood pressure response following the procedure. Patients in the two highest quartiles of daytime ambulatory systolic blood pressure at baseline exhibited significant ambulatory blood pressure reductions, whilst those in the lowest quartile exhibited little response.
To date, in excess of 10,000 patients worldwide have been treated with renal artery denervation [22]. Observational studies and open-label randomized controlled studies have suggested significant falls in blood pressure following treatment, with a particularly well-designed study (DENER-HTN) suggesting incremental benefit from RDN when applied over and above stepped anti-hypertensive therapy [9, 17, 23]. However, a randomized, sham-controlled trial (Symplicity HTN-3) failed to meet its primary efficacy endpoint, with blood pressure reductions in the denervated group matched by blood pressure falls in the sham-control arm [18].
There has been extensive commentary to date on the possible reasons why HTN-3 failed [22, 24, 25]. The first and most obvious reason is that the technology may be ineffective. However, the HTN-3 investigators have recently released data suggesting that the technique used in HTN-3 may have been sub-optimal, with only 6 % of subjects treated with the recommended bilateral retrograde spiral technique [19]. Clearly, sub-optimal denervation could have confounded the trial [26].
Other commentators have suggested that the failure of HTN-3 may have been catheter specific [27]. Further suggestion has been made of the role of ethnicity, the screening process, drug changes and lack of formal testing for drug adherence within that trial. These theories represent post hoc speculation in response to an unexpected negative result and therefore have to be considered with caution.
Sound physiological principles and surgical precedent underpin the field of RDN, which is operating in an area of medicine with substantial unmet need; the technology remains promising, appears safe [18, 28–30] and further randomized trials are required.
In this report, the UK Renal Denervation Affiliation details the results from 18 centers, each of which had performed more than five cases to date. Case selection was typically in accordance with the Joint UK Societies Consensus statement on RDN, which recommended strict criteria for patient selection [24]. These included: OSBP >160; systolic ASBP >150 on ≥3 antihypertensive agents (or in step 4 of the UK guideline [31]); exclusion of white-coat or secondary hypertension and patient selection by multidisciplinary teams of hypertension specialists and interventionists.
These data present a near-comprehensive national experience of the use of RDN technology, with over 85 % of experienced UK centers represented. The mean number of cases performed per center within this registry was 15 (SD 6.7). By comparison, the mean number of cases per center in HTN-3 was 4.1 [18].
Results show a fall in office BP of 22/9 mmHg at 11 months. Clearly, such data are open label and therefore have to be observed with caution, but this is a well screened and treated cohort, having previously been looked after by an average of 1.6 specialists with a named interest in hypertension. More than 85 % of subjects were managed in dedicated hypertension clinics prior to their denervation and relatively few drug increases were attempted after their procedure, despite the severity of their hypertension, suggesting a stable drug regimen was in place prior to their treatment.
Three times as many drugs were withdrawn following denervation as were added, with otherwise balanced dose-titrations observed across the cohort. This suggests that drug changes following RDN may have served to reduce the observed treatment effect of denervation, rather than magnify it. Clearly, however, whatever drug regimens were pursued, office blood pressure is prone to unconscious confounding, as described by others [32, 33]. Alternate methods of assessment of the success (or otherwise) of the technology are required.
Ambulatory blood pressure is a stronger predictor of outcome than office or home blood pressure readings and a better measure of true blood pressure than office readings. It is less prone to variability or confounding and makes pseudoresistant hypertension unlikely [34].
In this clinical cohort, a high proportion of patients were assessed using ABP. Some patients could not tolerate the repeated measures of ABP, which is understandable, given that some had very high blood pressures (office SBP >240) at the time of assessment. Despite this, follow-up ABP results were available in over 70 % of subjects.
Importantly, our cohort showed good pre-procedural approximation between office and ambulatory BP (pre-procedural office BP 186/102 mmHg; pre-procedural ABP of 170/98 mmHg) suggesting little white-coat element across the cohort.
Furthermore, subjects were prescribed an average of five medications at the time of their procedure, with a relatively high use (55 %) of aldosterone antagonists. To our knowledge, this is the highest proportion of subjects using aldosterone antagonists in any population of RDN patients reported to date. Despite these proactive drug strategies, mean pre-procedural daytime ABP remained 170/98 mmHg, which is, to our knowledge, as severe a cohort of hypertensives as have been studied with denervation to date.
Prior studies suggest an important role for aldosterone antagonism in the area of treatment-resistant hypertension [35]. The recently published PATHWAY-2 trial has confirmed spironolactone’s superior efficacy as a ‘step-four’ drug in hypertension pathways, when compared to B-Blockers and doxazosin. Furthermore, spironolactone has been proposed as an alternative to denervation, or a possible synergistic agent in blood pressure reduction following RDN [19, 36–38].
In this UK cohort of subjects, the use of aldosterone antagonists was not associated with a difference in blood pressure after RDN but this does not in any way question the efficacy of spironolactone in a resistant population. In this population, RDN was reserved for patients who were resistant to all recommended treatments and therefore we are observing a ‘treat to target’ effect, whereby other drugs are being used to compensate for the presence or absence of a spironolactone effect before a decision on RDN is made. Aldosterone antagonism use was not randomized within our cohort and therefore, by definition, the groups were not balanced and cannot be directly compared for efficacy of the drug. Rather, we report this to establish whether spironolactone acts as a predictor of blood pressure fall after RDN and it does not.
The pattern of ABP quartile response to RDN is an interesting finding from this study. The relationship between starting office blood pressure and magnitude of fall in BP has been previously described for office BP and we replicate this finding with our data. It has been suggested that this could represent a regression to the mean artefact, but ABPM is more resistant to that bias than office BP [39]. The large GLOBAL registry has also suggested an association of starting ABP with magnitude of fall in BP, but quartiles of response were not reported [29].
Given the strength of the association of fall in ASBP with ‘true’ starting BP observed in our cohort (as defined by daytime ASBP) these findings suggest that the most likely way to demonstrate the effectiveness of RDN in a randomized, blinded trial, where unconscious confounding of office response cannot bias the result and treatment effect sizes tend to be smaller [33], may be to test it in a cohort of patients with significant hypertension on ABP, rather than OBP.
Upcoming trials in the field of renal denervation have been proposed in patients with moderate hypertension (ABP of 140-170). Such patients most closely approximate to subjects in quartiles 1 and 2 of our study. Given that these trials are sham-controlled, we may expect to see results closer to those of daytime ABP, rather than open-label office pressure [32]. Rigorous control of potential confounders will therefore be important to pick up a true treatment effect size if these BP reductions are replicated.
Given the morbidity and mortality associated with uncontrolled hypertension, the need for treatment options over and above medications remains apparent, especially for those with few remaining medical options. Whilst we await further randomized trials in this area, results from this cohort of UK subjects with severe, treatment-resistant hypertension and few remaining medical options suggest that, on average, blood pressure control improved following RDN, especially in those with ambulatory blood pressure readings in the highest range.
Study limitations
This is an open-label retrospective registry with no outside funding source and therefore no independent verification of results was obtained. It is therefore limited by this study design. However, data quality appeared good, as supported by the relatively high frequency of reporting of ABP results and the close correlation between office BP and ABP results. Results also appear consistent across 18 sites.
This study did not mandate measures of adherence to prescribed medications and therefore variable levels of compliance pre- and post-procedure could have had a confounding impact on results. However, there is no reason to suspect changes in behavior occurred according to starting blood pressure and subjects within each quartile of starting ABP were prescribed similar numbers of pharmacological agents. Recent data have also shown blood pressure reductions after RDN in proven compliant subjects [40].
Future studies of RDN should, though, incorporate a direct assessment of adherence, such as urine antihypertensive drug analysis to look for confounding from variable drug compliance on results. Ultimately, however, novel measures of blood pressure reduction are needed for both adherent and non-adherent subjects and both these groups require study within separate, dedicated, randomized trials.
Reporting of ABP is not universal. ABP was tried in almost all patients within this cohort, but with a starting BP of >200 mmHg in many of these patients, the device was not tolerated for a 24-h period. Furthermore, many of these subjects travelled long distances to an RDN center for review and therefore repetition by the performing center was not feasible. Despite these limitations and the absence of reimbursement for RDN in the UK, 73 % use is a higher rate of use of ABP than in other funded registries to date.
Conclusion
This real-world study demonstrates that renal artery sympathetic denervation is associated with a significant reduction in both office and ambulatory blood pressure in well-characterized subjects with treatment-resistant hypertension.
Ambulatory blood pressure reductions were shown to be greatest in those with the highest starting ambulatory blood pressures, whilst those with blood pressures in the lowest quartile of baseline ambulatory blood pressure showed little response. Use of aldosterone antagonist did not affect the subsequent blood pressure response after denervation and drug changes after denervation did not appear to account for the blood pressure fall seen in the cohort at follow-up.
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J (2005) Global burden of hypertension: analysis of worldwide data. Lancet 365(9455):217–223
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M et al (2013) ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28):2159–2219
Campbell NR, Lackland DT, Niebylski ML (2014) World Hypertension League C, International Society of Hypertension Executive C. High blood pressure: why prevention and control are urgent and important—a 2014 fact sheet from the World Hypertension League and the International Society of Hypertension. J Clin Hypertens 16(8):551–553
de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P et al (2011) Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 57(5):898–902
Smithwick RH (1948) Continued hypertension; prognosis for surgically treated patients. Br Med J 2(4569):237–243
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K et al (2009) Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373(9671):1275–1281
Mahfoud F, Luscher TF, Andersson B, Baumgartner I, Cifkova R, Dimario C et al (2013) Expert consensus document from the European Society of Cardiology on catheter-based renal denervation. Eur Heart J 34(28):2149–2157
Symplicity HTNI (2011) Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 57(5):911–917
Esler MD, Bohm M, Sievert H, Rump CL, Schmieder RE, Krum H et al (2014) Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur Heart J 35(26):1752–1759
Dorr O, Liebetrau C, Mollmann H, Mahfoud F, Ewen S, Gaede L et al (2015) Beneficial effects of renal sympathetic denervation on cardiovascular inflammation and remodeling in essential hypertension. Clin Res Cardiol 104(2):175–184
Hilbert S, Rogge C, Papageorgiou P, Hindricks G, Bollmann A (2015) Successful single-sided renal denervation in drug-resistant hypertension and ventricular tachycardia. Clin Res Cardiol 104(3):279–281
Ott C, Harazny JM, Schmid A, Ditting T, Veelken R, Bladowski M et al (2015) Retinal microperfusion after renal denervation in treatment-resistant hypertensive patients. Clin Res Cardiol 104(9):782–789
Zhang M, Tao H, Shi KH (2015) Renal denervation as a friend of catheter ablation in patients with atrial fibrillation and hypertension. Clin Res Cardiol 104(1):85–86
Donazzan L, Mahfoud F, Ewen S, Ukena C, Cremers B, Kirsch CM et al (2015) Effects of catheter-based renal denervation on cardiac sympathetic activity and innervation in patients with resistant hypertension. Clin Res Cardiol. doi:10.1007/s00392-015-0930-4
Poss J, Ewen S, Schmieder RE, Muhler S, Vonend O, Ott C et al (2015) Effects of renal sympathetic denervation on urinary sodium excretion in patients with resistant hypertension. Clin Res Cardiol 104(8):672–678
Linz D, van Hunnik A, Ukena C, Ewen S, Mahfoud F, Schirmer SH et al (2014) Renal denervation: effects on atrial electrophysiology and arrhythmias. Clin Res Cardiol 103(10):765–774
Azizi M, Sapoval M, Gosse P, Monge M, Bobrie G, Delsart P et al. (2015) Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet 385(9981):1957–65
Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, Katzen BT et al (2014) A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370(15):1393–1401
Kandzari DE, Bhatt DL, Brar S, Devireddy CM, Esler M, Fahy M et al (2015) Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur Heart J 36(4):219–227
Caulfield M, de Belder M, Cleveland T et al. (2015) Joint UK Societies’ consensus summary statement on renal denervation for resistant hypertension. Heart 101(1):10–6
Symplicity HTNI, Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE et al (2010) Renal sympathetic denervation in patients with treatment-resistant hypertension (the symplicity HTN-2 trial): a randomised controlled trial. Lancet 376(9756):1903–1909
Mahfoud F, Bohm M, Azizi M, Pathak A, Durand Zaleski I, Ewen S et al. (2015) Proceedings from the European clinical consensus conference for renal denervation: considerations on future clinical trial design. Eur Heart J 36(33):2219–27
Krum H, Schlaich MP, Sobotka PA, Bohm M, Mahfoud F, Rocha-Singh K et al (2014) Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 383(9917):622–629
Lobo MD, de Belder MA, Cleveland T, Collier D, Dasgupta I, Deanfield J et al (2015) Joint UK societies’ 2014 consensus statement on renal denervation for resistant hypertension. Heart 101(1):10–16
Esler M (2014) Renal denervation for hypertension: observations and predictions of a founder. Eur Heart J 35(18):1178–1185
Mendelsohn FO (2014) Does complete renal denervation translate into superior clinical outcomes? Lessons learned from denervation of accessory renal arteries. Clin Res Cardiol 103(9):681–683
Mahfoud F, Luscher TF (2015) Renal denervation: symply trapped by complexity? Eur Heart J 36(4):199–202
Rippy MK, Zarins D, Barman NC, Wu A, Duncan KL, Zarins CK (2011) Catheter-based renal sympathetic denervation: chronic preclinical evidence for renal artery safety. Clin Res Cardiol 100(12):1095–1101
Bohm M, Mahfoud F, Ukena C, Hoppe UC, Narkiewicz K, Negoita M et al. (2015) First report of the Global SYMPLICITY Registry on the effect of renal artery denervation in patients with uncontrolled hypertension. Hypertension 65(4):766–74
Vogel B, Kirchberger M, Zeier M, Stoll F, Meder B, Saure D et al (2014) Renal sympathetic denervation therapy in the real world: results from the Heidelberg registry. Clin Res Cardiol 103(2):117–124
Excellence NIoHaC (2011) Hypertension: clinical management of primary hypertension in adults. NICE guideline CG 127
Howard JP, Francis DP (2014) Overcoming the three biases obscuring the science of renal denervation in humans: big-day bias, check-once-more bias and I-will-take-it-now bias. Trends Cardiovasc Med 25(2):116–8
Howard JP, Nowbar AN, Francis DP (2013) Size of blood pressure reduction from renal denervation: insights from meta-analysis of antihypertensive drug trials of 4121 patients with focus on trial design: the CONVERGE report. Heart 99(21):1579–1587
Niiranen TJ, Maki J, Puukka P, Karanko H, Jula AM (2014) Office, home, and ambulatory blood pressures as predictors of cardiovascular risk. Hypertension 64(2):281–286
Chapman N, Dobson J, Wilson S, Dahlof B, Sever PS, Wedel H et al (2007) Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension 49(4):839–845
Rosa J, Widimsky P, Tousek P, Petrak O, Curila K, Waldauf P et al (2015) Randomized comparison of renal denervation versus intensified pharmacotherapy including spironolactone in true-resistant hypertension: six-month results from the prague-15 study. Hypertension 65(2):407–413
Mahfoud F, Ruilope LM, Bohm M, Schmieder RE (2015) Aldosterone antagonists and renal denervation: friends or foes? Hypertension 65(2):280–282
Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G et al. (2015) Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet 386(10008):2059–68
Howard JP, Cole GD, Sievert H, Bhatt DL, Papademetriou V, Kandzari DE et al (2014) Unintentional overestimation of an expected antihypertensive effect in drug and device trials: mechanisms and solutions. Int J Cardiol 172(1):29–35
Ewen S, Meyer MR, Cremers B, Laufs U, Helfer AG, Linz D et al. (2015) Blood pressure reductions following catheter-based renal denervation are not related to improvements in adherence to antihypertensive drugs measured by urine/plasma toxicological analysis. Clin Res Cardiol 104(12):1097–105
Acknowledgments
A list of contributing co-investigators in included in supplementary material (Online Appendix 1). Dr A. Sharp would like to acknowledge support from the Gawthorn Cardiac Trust and the Exeter National Institute of Health Research Clinical Research Facility. Dr M. Lobo and Professor M Caulfield would like to acknowledge support from Bart’s Charitable Fund and the UK National Institute of Health Research for institutional support. Professor Caulfield is an NIHR senior investigator. Dr A. Nightingale and Professor Baumbach would like to acknowledge the UK National Institute of Health Research for institutional support. Dr Sharp is a consultant for and reports research funding from Medtronic Inc. Dr Davies is a consultant for Medtronic and Recor Medical; he has received research funding from Medtronic Inc. Dr Lobo is a consultant and speaker for ROX medical, Medtronic and St Jude Medical; he also speaks for Cardiosonic. He reports educational grants from Medtronic Inc. Dr Dasgupta reports research funding from Medtronic Inc. Dr McKane reports speaking honoraria for Medtronic Inc and has been a consultant for St Jude Medical. Dr Gerber is a consultant for Medtronic Inc. Professor Caulfield has previously received honoraria from Medtronic Inc. Dr Thackray would like to acknowledge Hull & East Riding Cardiac Trust Fund and Hull PCT for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Sources of funding
No funding was sought or received for this study.
Additional information
On behalf of the UK Renal Denervation affiliation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sharp, A.S.P., Davies, J.E., Lobo, M.D. et al. Renal artery sympathetic denervation: observations from the UK experience. Clin Res Cardiol 105, 544–552 (2016). https://doi.org/10.1007/s00392-015-0959-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0959-4