Abstract
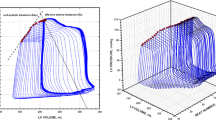
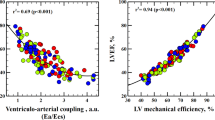
In animal experiments, elevating systolic pressures induces diastolic dysfunction and may contribute to congestion, a finding not yet translated to humans. Coronary surgery patients (63 ± 8 years) were studied with left ventricular (LV) pressure (n = 17) or pressure–volume (n = 3) catheters, immediately before cardiopulmonary bypass. Single-beat graded pressure elevations were induced by clamping the ascending aorta. Protocol was repeated after volume loading (n = 7). Consecutive patients with a wide range of systolic function were included. Peak isovolumetric LV pressure (LVPiso) ranged from 113 to 261 mmHg. With preserved systolic function, LVP elevations neither delayed relaxation nor increased filling pressures. With decreasing systolic function, diastolic tolerance to afterload progressively disappeared: relaxation slowed and filling pressures increased (diastolic dysfunction). In severely depressed systolic function, filling pressures increased even with minor LVP elevations, suggesting baseline load-dependent elevation of diastolic pressures. The magnitude of filling pressure elevation induced in isovolumetric heartbeats was closely and inversely related to systolic performance, evaluated by LVPiso (r = −0.96), and directly related to changes in the time constant of relaxation τ (r = 0.95). The maximum tolerated systolic LVP (without diastolic dysfunction) was similarly correlated with LVPiso (r = 0.99). Volume loading itself accelerated relaxation, but augmented afterload-induced upward shift of filling pressures (7.9 ± 3.7 vs. 3.0 ± 1.5; P < 0.01). The normal human response to even markedly increased systolic pressures is no slowing of relaxation and preservation of normal filling pressures. When cardiac function deteriorates, the LV becomes less tolerant, responding with slowed relaxation and increased filling pressures. This increase is exacerbated by volume loading.





Similar content being viewed by others
References
Atherton JJ, Moore TD, Lele SS, Thomson HL, Galbraith AJ, Belenkie I, Tyberg JV, Frenneaux MP (1997) Diastolic ventricular interaction in chronic heart failure. Lancet 349:1720–1724. doi:10.1016/S0140-6736(96)05109-4
Borbely A, Papp Z, Edes I, Paulus WJ (2009) Molecular determinants of heart failure with normal left ventricular ejection fraction. Pharmacol Rep. 61:139–145
Borlaug BA, Kass DA (2008) Ventricular–vascular interaction in heart failure. Heart Fail Clin 4:23–36. doi:10.1016/j.hfc.2007.10.001
Borlaug BA, Lam CS, Roger VL, Rodeheffer RJ, Redfield MM (2009) Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J Am Coll Cardiol 54:410–418. doi:10.1016/j.jacc.2009.05.013
Borlaug BA, Melenovsky V, Redfield MM, Kessler K, Chang HJ, Abraham TP, Kass DA (2007) Impact of arterial load and loading sequence on left ventricular tissue velocities in humans. J Am Coll Cardiol 50:1570–1577. doi:10.1016/j.jacc.2007.07.032
Burkhoff D, Sagawa K (1986) Ventricular efficiency predicted by an analytical model. Am J Physiol 250:R1021–R1027
Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA (1998) Coupled systolic-ventricular and vascular stiffening with age: implications for pressure regulation and cardiac reserve in the elderly. J Am Coll Cardiol 32:1221–1227. doi:10.1016/S0735-1097(98)00374-X
Correia-Pinto J, Henriques-Coelho T, Roncon-Albuquerque R Jr, Lourenco AP, Melo-Rocha G, Vasques-Novoa F, Gillebert TC, Leite-Moreira AF (2009) Time course and mechanisms of left ventricular systolic and diastolic dysfunction in monocrotaline-induced pulmonary hypertension. Basic Res Cardiol 104:535–545. doi:10.1007/s00395-009-0017-3
De Hert SG, Gillebert TC, Ten Broecke PW, Mertens E, Rodrigus IE, Moulijn AC (1999) Contraction–relaxation coupling and impaired left ventricular performance in coronary surgery patients. Anesthesiology 90:748–757. doi:10.1097/00000542-199903000-00017
Eichhorn EJ, Willard JE, Alvarez L, Kim AS, Glamann DB, Risser RC, Grayburn PA (1992) Are contraction and relaxation coupled in patients with and without congestive heart failure? Circulation 85:2132–2139. doi:10.1161/01.CIR.85.6.2132
Falcao-Pires I, Palladini G, Goncalves N, van der Velden J, Moreira-Goncalves D, Miranda-Silva D, Salinaro F, Paulus WJ, Niessen HW, Perlini S, Leite-Moreira AF (2011) Distinct mechanisms for diastolic dysfunction in diabetes mellitus and chronic pressure-overload. Basic Res Cardiol 106:801–814. doi:10.1007/s00395-011-0184-x
Fukuta H, Little WC (2008) The cardiac cycle and the physiologic basis of left ventricular contraction, ejection, relaxation, and filling. Heart Fail Clin 4:1–11. doi:10.1016/j.hfc.2007.10.004
Gaasch WH, Delorey DE, Kueffer FJ, Zile MR (2009) Distribution of left ventricular ejection fraction in patients with ischemic and hypertensive heart disease and chronic heart failure. Am J Cardiol 104:1413–1415. doi:10.1016/j.amjcard.2009.06.064
Gaasch WH, Little WC (2007) Assessment of left ventricular diastolic function and recognition of diastolic heart failure. Circulation 116:591–593. doi:10.1161/CIRCULATIONAHA.107.716647
Gaasch WH, Zile MR (2004) Left ventricular diastolic dysfunction and diastolic heart failure. Annu Rev Med 55:373–394. doi:10.1146/annurev.med.55.091902.104417
Galderisi M, Cicala S, Caso P, De Simone L, D’Errico A, Petrocelli A, de Divitiis O (2002) Coronary flow reserve and myocardial diastolic dysfunction in arterial hypertension. Am J Cardiol 90:860–864. doi:10.1016/S0002-9149(02)02708-X
Gandhi SK, Powers JC, Nomeir AM, Fowle K, Kitzman DW, Rankin KM, Little WC (2001) The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 344:17–22. doi:10.1056/NEJM200101043440103
Gelpi RJ, Pasipoularides A, Lader AS, Patrick TA, Chase N, Hittinger L, Shannon RP, Bishop SP, Vatner SF (1991) Changes in diastolic cardiac function in developing and stable perinephritic hypertension in conscious dogs. Circ Res 68:555–567. doi:10.1161/01.RES.68.2.555
Gillebert TC, Leite-Moreira AF, De Hert SG (1997) Relaxation-systolic pressure relation. A load-independent assessment of left ventricular contractility. Circulation 95:745–752. doi:10.1161/01.CIR.95.3.745
Grossman W (2000) Defining diastolic dysfunction. Circulation. 101:2020–2021
Heusch G (2009) Diastolic heart failure: a misNOmer. Basic Res Cardiol 104:465–467. doi:10.1007/s00395-009-0025-3
Ishizaka S, Asanoi H, Wada O, Kameyama T, Inoue H (1995) Loading sequence plays an important role in enhanced load sensitivity of left ventricular relaxation in conscious dogs with tachycardia-induced cardiomyopathy. Circulation 92:3560–3567. doi:10.1161/01.CIR.92.12.3560
Ladeiras-Lopes R, Ferreira-Martins J, Leite-Moreira AF (2009) Acute neurohumoral modulation of diastolic function. Peptides 30:419–425. doi:10.1016/j.peptides.2008.10.018
Leite-Moreira AF, Correia-Pinto J (2001) Load as an acute determinant of end-diastolic pressure–volume relation. Am J Physiol Heart Circ Physiol 280:H51–H59
Leite-Moreira AF, Correia-Pinto J, Gillebert TC (1999) Afterload induced changes in myocardial relaxation: a mechanism for diastolic dysfunction. Cardiovasc Res 43:344–353. doi:10.1016/S0008-6363(99)00099-1
Leite-Moreira AF, Gillebert TC (1994) Nonuniform course of left ventricular pressure fall and its regulation by load and contractile state. Circulation 90:2481–2491. doi:10.1161/01.CIR.90.5.2481
Leite-Moreira AF, Gillebert TC (1996) Myocardial relaxation in regionally stunned left ventricle. Am J Physiol 270:H509–H517
MacIver DH (2010) Is remodeling the dominant compensatory mechanism in both chronic heart failure with preserved and reduced left ventricular ejection fraction? Basic Res Cardiol 105:227–234. doi:10.1007/s00395-009-0063-x
Mann DL, Bristow MR (2005) Mechanisms and models in heart failure: the biomechanical model and beyond. Circulation 111:2837–2849. doi:10.1161/CIRCULATIONAHA.104.500546
Matsubara H, Takaki M, Yasuhara S, Araki J, Suga H (1995) Logistic time constant of isovolumic relaxation pressure–time curve in the canine left ventricle. Better alternative to exponential time constant. Circulation 92:2318–2326. doi:10.1161/01.CIR.92.8.2318
Munagala VK, Hart CY, Burnett JC Jr, Meyer DM, Redfield MM (2005) Ventricular structure and function in aged dogs with renal hypertension: a model of experimental diastolic heart failure. Circulation 111:1128–1135. doi:10.1161/01.CIR.0000157183.21404.63
Opdahl A, Remme EW, Helle-Valle T, Lyseggen E, Vartdal T, Pettersen E, Edvardsen T, Smiseth OA (2009) Determinants of left ventricular early-diastolic lengthening velocity: independent contributions from left ventricular relaxation, restoring forces, and lengthening load. Circulation 119:2578–2586. doi:10.1161/CIRCULATIONAHA.108.791681
Paulus WJ, Grossman W, Serizawa T, Bourdillon PD, Pasipoularides A, Mirsky I (1985) Different effects of two types of ischemia on myocardial systolic and diastolic function. Am J Physiol 248:H719–H728
Raff GL, Glantz SA (1981) Volume loading slows left ventricular isovolumic relaxation rate. Evidence of load-dependent relaxation in the intact dog heart. Circ Res 48:813–824. doi:10.1161/01.RES.48.6.813
Ritter M, Hess OM, Murakami T, Jenni R, Egloff L, Nonogi H, Schneider J, Krayenbuehl HP (1988) Left ventricular systolic series elastic properties in aortic stenosis before and after valve replacement. Cardiovasc Res 22:759–767. doi:10.1093/cvr/22.11.759
Schulz R, Rose J, Post H, Skyschally A, Heusch G (2000) Less afterload sensitivity in short-term hibernating than in acutely ischemic and stunned myocardium. Am J Physiol Heart Circ Physiol 279:H1106–H1110
Senzaki H, Kass DA (2009) Analysis of isovolumic relaxation in failing hearts by monoexponential time constants overestimates lusitropic change and load dependence: mechanisms and advantages of alternative logistic fit. Circ Heart Fail 3:268–276. doi:10.1161/CIRCHEARTFAILURE.109.865592
Sossalla S, Maurer U, Schotola H, Hartmann N, Didie M, Zimmermann WH, Jacobshagen C, Wagner S, Maier LS (2011) Diastolic dysfunction and arrhythmias caused by overexpression of CaMKIIdelta(C) can be reversed by inhibition of late Na(+) current. Basic Res Cardiol 106:263–272. doi:10.1007/s00395-010-0136-x
Suga H (1990) Ventricular energetics. Physiol Rev 70:247–277
Westermann D, Riad A, Richter U, Jager S, Savvatis K, Schuchardt M, Bergmann N, Tolle M, Nagorsen D, Gotthardt M, Schultheiss HP, Tschope C (2009) Enhancement of the endothelial NO synthase attenuates experimental diastolic heart failure. Basic Res Cardiol 104:499–509. doi:10.1007/s00395-009-0014-6
Yip G, Wang M, Zhang Y, Fung JW, Ho PY, Sanderson JE (2002) Left ventricular long axis function in diastolic heart failure is reduced in both diastole and systole: time for a redefinition? Heart 87:121–125. doi:10.1136/heart.87.2.121
Acknowledgments
This work was supported by the Portuguese Foundation for Science and Technology (grant number PIC/IC/82943/2007), through the Cardiovascular R&D Unit (nr. 51/94) and by a grant from the European Commission (FP7-Health-2010; MEDIA-261409).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leite-Moreira, A.F., Lourenço, A.P., Roncon-Albuquerque, R. et al. Diastolic tolerance to systolic pressures closely reflects systolic performance in patients with coronary heart disease. Basic Res Cardiol 107, 251 (2012). https://doi.org/10.1007/s00395-012-0251-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-012-0251-y