Abstract
Objectives
Despite advances in our understanding of metabolic syndrome (MetS) and the treatment of each of its components separately, currently there is no single therapy approved to manage it as a single condition. Since multi-drug treatment increases drug interactions, decreases patient compliance and increases health costs, it is important to introduce single therapies that improve all of the MetS components.
Evidence acquisition
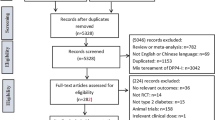
We conducted a PubMed, Scopus, Google Scholar, Web of Science, US FDA, utdo.ir and clinicaltrial.gov search, gathered the most relevant preclinical and clinical studies that have been published since 2010, and discussed the beneficial effects of dipeptidyl peptidase (DPP)-4 inhibitors to prevent and treat different constituent of the MetS as a single therapy. Furthermore, the pharmacology of DPP-4 inhibitors, focusing on pharmacodynamics, pharmacokinetics, drug interactions and their side effects are also reviewed.
Results
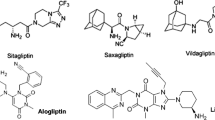
DPP-4 inhibitors or gliptins are a new class of oral anti-diabetic drugs that seem safe drugs with no severe side effects, commonly GI disturbance, infection and inflammatory bowel disease. They increase mass and function of pancreatic β-cells, and insulin sensitivity in liver, muscle and adipose tissue. It has been noted that gliptin therapy decreases dyslipidemia. DPP-4 inhibitors increase fatty oxidation, and cholesterol efflux, and decrease hepatic triglyceride synthase and de novo lipogenesis. They delay gastric emptying time and lead to satiety. Besides, gliptin therapy has anti-inflammatory and anti-atherogenic impacts, and improves endothelial function and reduces vascular stiffness.
Conclusion
The gathered data prove the efficacy of DPP-4 inhibitors in managing MetS in some levels beyond anti-diabetic effects. This review could be a lead for designing new DPP-4 inhibitors with greatest effects on MetS in future. Introducing drugs with polypharmacologic effects could increase the patient’s compliance and decrease the health cost that there is not in multi-drug therapy.

ᅟ


Similar content being viewed by others
Abbreviations
- cAMP:
-
cyclic adenosine monophosphate
- DPP-4:
-
dipeptidyl peptidase
- eNOS:
-
endothelial NO synthesize
- FBS:
-
fasting blood sugar
- FDA:
-
US Food and Drug Administration
- GIP:
-
gastric inhibitory polypeptide
- GLP-1:
-
glucagon-like peptide
- HbA1c:
-
hemoglobin A1c
- HDL-C:
-
high-density lipoprotein cholesterol
- IDL-C:
-
intermediate density lipoprotein cholesterol
- LDL-C:
-
low-density lipoprotein cholesterol
- P-gp:
-
P-glycoprotein
- t 1/2 :
-
half-life
- T1D:
-
type 1 diabetes
- T2DM:
-
type 2 diabetes mellitus
- VLDL-C:
-
very-low-density lipoprotein cholesterol
References
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20(2):12. https://doi.org/10.1007/s11906-018-0812-z.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735–52. https://doi.org/10.1161/circulationaha.105.169404.
Masoudi-Kazemabad A, Jamialahmadi K, Moohebati M, Mojarrad M, Manshadi RD, Akhlaghi S, et al. Neuropeptide y Leu7Pro polymorphism associated with the metabolic syndrome and its features in patients with coronary artery disease. Angiology. 2013;64(1):40–5. https://doi.org/10.1177/0003319711435149.
Khayyatzadeh SS, Moohebati M, Mazidi M, Avan A, Tayefi M, Parizadeh SMR, et al. Nutrient patterns and their relationship to metabolic syndrome in Iranian adults. Eur J Clin Investig. 2016;46(10):840–52. https://doi.org/10.1111/eci.12666.
Stojanoska MM, Milosevic N, Milic N, Abenavoli L. The influence of phthalates and bisphenol a on the obesity development and glucose metabolism disorders. Endocrine. 2017;55(3):666–81. https://doi.org/10.1007/s12020-016-1158-4.
Baghshini MR, Nikbakht-Jam I, Mohaddes-Ardabili H, Pasdar A, Avan A, Tayefi M, et al. Higher prevalence of metabolic syndrome among male employees of a gas refinery than in their counterparts in nonindustrial environments. Asian Biomedicine. 2017;11(3):227–34. https://doi.org/10.5372/1905-7415.1103.553.
Rask Larsen J, Dima L, Correll CU, Manu P. The pharmacological management of metabolic syndrome. Expert Rev Clin Pharmacol. 2018;11(4):397–410. https://doi.org/10.1080/17512433.2018.1429910.
Martin KA, Mani MV, Mani A. New targets to treat obesity and the metabolic syndrome. Eur J Pharmacol. 2015;763(Pt A):64–74. https://doi.org/10.1016/j.ejphar.2015.03.093.
Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology. 2007;132(6):2131–57. https://doi.org/10.1053/j.gastro.2007.03.054.
Yazbeck R, Howarth GS, Abbott CA. Dipeptidyl peptidase inhibitors, an emerging drug class for inflammatory disease? Trends Pharmacol Sci. 2009;30(11):600–7. https://doi.org/10.1016/j.tips.2009.08.003.
Seino Y, Fukushima M, Yabe D. GIP and GLP-1, the two incretin hormones: similarities and differences. J Diabetes Investig. 2010;1(1–2):8–23. https://doi.org/10.1111/j.2040-1124.2010.00022.x.
Barber TM, Begbie H, Levy J. The incretin pathway as a new therapeutic target for obesity. Maturitas. 2010;67(3):197–202. https://doi.org/10.1016/j.maturitas.2010.06.018.
Drucker DJ, Rosen CF. Glucagon-like peptide-1 (GLP-1) receptor agonists, obesity and psoriasis: diabetes meets dermatology. Diabetologia. 2011;54(11):2741–4. https://doi.org/10.1007/s00125-011-2297-z.
Nistala R, Savin V. Diabetes, hypertension, and chronic kidney disease progression: role of DPP4. Am J Physiol Renal Physiol. 2017;312(4):F661–F70. https://doi.org/10.1152/ajprenal.00316.2016.
Razavi BM, Hosseinzadeh H. Saffron: a promising natural medicine in the treatment of metabolic syndrome. J Sci Food Agric. 2017;97(6):1679–85. https://doi.org/10.1002/jsfa.8134.
Razavi BM, Lookian F, Hosseinzadeh H. Protective effects of green tea on olanzapine-induced-metabolic syndrome in rats. Biomed Pharmacother. 2017;92:726–31. https://doi.org/10.1016/j.biopha.2017.05.113.
Tabeshpour J, Imenshahidi M, Hosseinzadeh H. A review of the effects of berberis vulgaris and its major component, berberine, in metabolic syndrome. Iran J Basic Med Sci. 2017;20(5):557–68. https://doi.org/10.22038/ijbms.2017.8682.
Tabeshpour J, Razavi BM, Hosseinzadeh H. Effects of avocado (Persea americana) on metabolic syndrome: a comprehensive systematic review. Phytother Res. 2017;31(6):819–37. https://doi.org/10.1002/ptr.5805.
Mazidi M, Rezaie P, Kengne AP, Mobarhan MG, Ferns GA. Gut microbiome and metabolic syndrome. Diabetes Metab Syndr Clin Res Rev. 2016;10(2):S150–S7. https://doi.org/10.1016/j.dsx.2016.01.024.
Sattigeri JA, Sethi S, Davis JA, Ahmed S, Rayasam GV, Jadhav BG, et al. Approaches towards the development of chimeric DPP4/ACE inhibitors for treating metabolic syndrome. Bioorg Med Chem Lett. 2017;27(11):2313–8. https://doi.org/10.1016/j.bmcl.2017.04.036.
Jackson EK. Dipeptidyl peptidase IV inhibition alters the hemodynamic response to angiotensin-converting enzyme inhibition in humans with the metabolic syndrome. Hypertension. 2010;56(4):581–3. https://doi.org/10.1161/hypertensionaha.110.158527.
Marney A, Kunchakarra S, Byrne L, Brown NJ. Interactive hemodynamic effects of dipeptidyl peptidase-IV inhibition and angiotensin-converting enzyme inhibition in humans. Hypertension. 2010;56(4):728–33. https://doi.org/10.1161/hypertensionaha.110.156554.
Baetta R, Corsini A. Pharmacology of dipeptidyl peptidase-4 inhibitors: similarities and differences. Drugs. 2011;71(11):1441–67. https://doi.org/10.2165/11591400-000000000-00000.
Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest. 1993;91(1):301–7. https://doi.org/10.1172/jci116186.
Wang Q, Long M, Qu H, Shen R, Zhang R, Xu J, et al. DPP-4 inhibitors as treatments for type 1 diabetes mellitus: a systematic review and meta-analysis. J Diabetes Res. 2018;2018:10. https://doi.org/10.1155/2018/5308582.
De Silva A, Bloom SR. Gut hormones and appetite control: a focus on PYY and GLP-1 as therapeutic targets in obesity. Gut Liver. 2012;6(1):10–20. https://doi.org/10.5009/gnl.2012.6.1.10.
Scheen AJ. The safety of gliptins : updated data in 2018. Expert Opin Drug Saf. 2018;17(4):387–405. https://doi.org/10.1080/14740338.2018.1444027.
Deacon CF, Lebovitz HE. Comparative review of dipeptidyl peptidase-4 inhibitors and sulphonylureas. Diabetes Obes Metab. 2016;18(4):333–47. https://doi.org/10.1111/dom.12610.
Choy M, Lam S. Sitagliptin: a novel drug for the treatment of type 2 diabetes. Cardiol Rev. 2007;15(5):264–71. https://doi.org/10.1097/CRD.0b013e318123f771.
McCormack PL. Evogliptin: first global approval. Drugs. 2015;75(17):2045–9. https://doi.org/10.1007/s40265-015-0496-5.
Kadowaki T, Kondo K. Efficacy, safety and dose-response relationship of teneligliptin, a dipeptidyl peptidase-4 inhibitor, in Japanese patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2013;15(9):810–8. https://doi.org/10.1111/dom.12092.
Sheu WH, Gantz I, Chen M, Suryawanshi S, Mirza A, Goldstein BJ, et al. Safety and efficacy of Omarigliptin (MK-3102), a novel once-weekly DPP-4 inhibitor for the treatment of patients with type 2 diabetes. Diabetes Care. 2015;38(11):2106–14. https://doi.org/10.2337/dc15-0109.
Deacon CF. Dipeptidyl peptidase 4 inhibition with sitagliptin: a new therapy for type 2 diabetes. Expert Opin Investig Drugs. 2007;16(4):533–45. https://doi.org/10.1517/13543784.16.4.533.
Karagiannis T, Boura P, Tsapas A. Safety of dipeptidyl peptidase 4 inhibitors: a perspective review. Ther Adv Drug Saf. 2014;5(3):138–46. https://doi.org/10.1177/2042098614523031.
Tofovic DS, Bilan VP, Jackson EK. Sitagliptin augments angiotensin II-induced renal vasoconstriction in kidneys from rats with metabolic syndrome. Clin Exp Pharmacol Physiol. 2010;37(7):689–91. https://doi.org/10.1111/j.1440-1681.2010.05389.x.
Aschner P, Kipnes MS, Lunceford JK, Sanchez M, Mickel C, Williams-Herman DE. Effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care. 2006;29(12):2632–7. https://doi.org/10.2337/dc06-0703.
Traynor K. FDA approves saxagliptin for type 2 diabetes. Am J Health Syst Pharm. 2009;66(17):1513. https://doi.org/10.2146/news090069.
Rosenstock J, Aguilar-Salinas C, Klein E, Nepal S, List J, Chen R. Effect of saxagliptin monotherapy in treatment-naive patients with type 2 diabetes. Curr Med Res Opin. 2009;25(10):2401–11. https://doi.org/10.1185/03007990903178735.
Lam S, Saad M. Saxagliptin: a new dipeptidyl peptidase-4 inhibitor for type 2 diabetes. Cardiol Rev. 2010;18(4):213–7. https://doi.org/10.1097/CRD.0b013e3181daad5f.
Aletti R, Cheng-Lai A. Linagliptin: the newest dipeptidyl peptidase-4 inhibitor for type 2 diabetes mellitus. Cardiol Rev. 2012;20(1):45–51. https://doi.org/10.1097/CRD.0b013e31823a3afc.
Del Prato S, Barnett AH, Huisman H, Neubacher D, Woerle HJ, Dugi KA. Effect of linagliptin monotherapy on glycaemic control and markers of beta-cell function in patients with inadequately controlled type 2 diabetes: a randomized controlled trial. Diabetes Obes Metab. 2011;13(3):258–67. https://doi.org/10.1111/j.1463-1326.2010.01350.x.
Marino AB, Cole SW. Alogliptin: safety, efficacy, and clinical implications. J Pharm Pract. 2015;28(1):99–106. https://doi.org/10.1177/0897190014522063.
Covington P, Christopher R, Davenport M, Fleck P, Mekki QA, Wann ER, et al. Pharmacokinetic, pharmacodynamic, and tolerability profiles of the dipeptidyl peptidase-4 inhibitor alogliptin: a randomized, double-blind, placebo-controlled, multiple-dose study in adult patients with type 2 diabetes. Clin Ther. 2008;30(3):499–512. https://doi.org/10.1016/j.clinthera.2008.03.004.
Chen XW, He ZX, Zhou ZW, Yang T, Zhang X, Yang YX, et al. An update on the clinical pharmacology of the dipeptidyl peptidase 4 inhibitor alogliptin used for the treatment of type 2 diabetes mellitus. Clin Exp Pharmacol Physiol. 2015;42(12):1225–38. https://doi.org/10.1111/1440-1681.12469.
Pi-Sunyer FX, Schweizer A, Mills D, Dejager S. Efficacy and tolerability of vildagliptin monotherapy in drug-naive patients with type 2 diabetes. Diabetes Res Clin Pract. 2007;76(1):132–8. https://doi.org/10.1016/j.diabres.2006.12.009.
Kim SH, Lee SH, Yim HJ. Gemigliptin, a novel dipeptidyl peptidase 4 inhibitor: first new anti-diabetic drug in the history of Korean pharmaceutical industry. Arch Pharm Res. 2013;36(10):1185–8. https://doi.org/10.1007/s12272-013-0171-x.
Gutch M, Joshi A, Kumar S, Agarwal A, Pahan RK, Razi SM. Gemigliptin: newer promising gliptin for type 2 diabetes mellitus. Indian J Endocr Metab. 2017;21(6):898–902. https://doi.org/10.4103/ijem.IJEM_20_17.
Nishio S, Abe M, Ito H. Anagliptin in the treatment of type 2 diabetes: safety, efficacy, and patient acceptability. Diabetes Metab Syndr Obes. 2015;8:163–71. https://doi.org/10.2147/dmso.s54679.
Gu N, Park MK, Kim TE, Bahng MY, Lim KS, Cho SH, et al. Multiple-dose pharmacokinetics and pharmacodynamics of evogliptin (DA-1229), a novel dipeptidyl peptidase IV inhibitor, in healthy volunteers. Drug Des Devel Ther. 2014;8:1709–21. https://doi.org/10.2147/DDDT.S65678.
Park J, Park SW, Yoon KH, Kim SR, Ahn KJ, Lee JH, et al. Efficacy and safety of evogliptin monotherapy in patients with type 2 diabetes and moderately elevated glycated haemoglobin levels after diet and exercise. Diabetes Obes Metab. 2017;19(12):1681–7. https://doi.org/10.1111/dom.12987.
Burness CB. Omarigliptin: first global approval. Drugs. 2015;75(16):1947–52. https://doi.org/10.1007/s40265-015-0493-8.
Xu S, Tatosian D, McIntosh I, Caceres M, Matthews C, Samuel K, et al. Absorption, metabolism and excretion of [(14)C]omarigliptin, a once-weekly DPP-4 inhibitor, in humans. Xenobiotica. 2018;48(6):584–91. https://doi.org/10.1080/00498254.2017.1346333.
McKeage K. Trelagliptin: first global approval. Drugs. 2015;75(10):1161–4. https://doi.org/10.1007/s40265-015-0431-9.
Kaku K. First novel once-weekly DPP-4 inhibitor, trelagliptin, for the treatment of type 2 diabetes mellitus. Expert Opin Pharmacother. 2015;16(16):2539–47. https://doi.org/10.1517/14656566.2015.1099630.
Nakamaru Y, Hayashi Y, Ikegawa R, Kinoshita S, Perez Madera B, Gunput D, et al. Metabolism and disposition of the dipeptidyl peptidase IV inhibitor teneligliptin in humans. Xenobiotica. 2014;44(3):242–53. https://doi.org/10.3109/00498254.2013.816891.
Morishita R, Nakagami H. Teneligliptin : expectations for its pleiotropic action. Expert Opin Pharmacother. 2015;16(3):417–26. https://doi.org/10.1517/14656566.2015.1000301.
Furuta S, Smart C, Hackett A, Benning R, Warrington S. Pharmacokinetics and metabolism of [14C]anagliptin, a novel dipeptidyl peptidase-4 inhibitor, in humans. Xenobiotica. 2013;43(5):432–42. https://doi.org/10.3109/00498254.2012.731618.
Graefe-Mody U, Retlich S, Friedrich C. Clinical pharmacokinetics and pharmacodynamics of linagliptin. Clin Pharmacokinet. 2012;51(7):411–27. https://doi.org/10.2165/11630900-000000000-00000.
Heise T, Graefe-Mody EU, Huttner S, Ring A, Trommeshauser D, Dugi KA. Pharmacokinetics, pharmacodynamics and tolerability of multiple oral doses of linagliptin, a dipeptidyl peptidase-4 inhibitor in male type 2 diabetes patients. Diabetes Obes Metab. 2009;11(8):786–94. https://doi.org/10.1111/j.1463-1326.2009.01046.x.
Anderson R, Hayes J, Stephens JW. Pharmacokinetic, pharmacodynamic and clinical evaluation of saxagliptin in type 2 diabetes. Expert Opin Drug Metab Toxicol. 2016;12(4):467–73. https://doi.org/10.1517/17425255.2016.1154044.
Vincent SH, Reed JR, Bergman AJ, Elmore CS, Zhu B, Xu S, et al. Metabolism and excretion of the dipeptidyl peptidase 4 inhibitor [14C]sitagliptin in humans. Drug Metab Dispos. 2007;35(4):533–8. https://doi.org/10.1124/dmd.106.013136.
Bergman AJ, Stevens C, Zhou Y, Yi B, Laethem M, De Smet M, et al. Pharmacokinetic and pharmacodynamic properties of multiple oral doses of sitagliptin, a dipeptidyl peptidase-IV inhibitor: a double-blind, randomized, placebo-controlled study in healthy male volunteers. Clin Ther. 2006;28(1):55–72. https://doi.org/10.1016/j.clinthera.2006.01.015.
He YL, Wang Y, Bullock JM, Deacon CF, Holst JJ, Dunning BE, et al. Pharmacodynamics of vildagliptin in patients with type 2 diabetes during OGTT. J Clin Pharmacol. 2007;47(5):633–41. https://doi.org/10.1177/0091270006299137.
He H, Tran P, Yin H, Smith H, Batard Y, Wang L, et al. Absorption, metabolism, and excretion of [14C]vildagliptin, a novel dipeptidyl peptidase 4 inhibitor, in humans. Drug Metab Dispos. 2009;37(3):536–44. https://doi.org/10.1124/dmd.108.023010.
Krishna R, Bergman A, Larson P, Cote J, Lasseter K, Dilzer S, et al. Effect of a single cyclosporine dose on the single-dose pharmacokinetics of sitagliptin (MK-0431), a dipeptidyl peptidase-4 inhibitor, in healthy male subjects. J Clin Pharmacol. 2007;47(2):165–74. https://doi.org/10.1177/0091270006296523.
Abrahami D, Douros A, Yin H, Yu OHY, Renoux C, Bitton A, et al. Dipeptidyl peptidase-4 inhibitors and incidence of inflammatory bowel disease among patients with type 2 diabetes: population based cohort study. Br Med J. 2018;360:k872. https://doi.org/10.1136/bmj.k872.
Srikanth S, Deedwania P. Management of Dyslipidemia in patients with hypertension, diabetes, and metabolic syndrome. Curr Hypertens Rep. 2016;18(10):76. https://doi.org/10.1007/s11906-016-0683-0.
Ervinna N, Mita T, Yasunari E, Azuma K, Tanaka R, Fujimura S, et al. Anagliptin, a DPP-4 inhibitor, suppresses proliferation of vascular smooth muscles and monocyte inflammatory reaction and attenuates atherosclerosis in male apo e-deficient mice. Endocrinology. 2013;154(3):1260–70. https://doi.org/10.1210/en.2012-1855.
Ta NN, Schuyler CA, Li Y, Lopes-Virella MF, Huang Y. DPP-4 (CD26) inhibitor alogliptin inhibits atherosclerosis in diabetic apolipoprotein E-deficient mice. J Cardiovasc Pharmacol. 2011;58(2):157–66. https://doi.org/10.1097/FJC.0b013e31821e5626.
Yano W, Inoue N, Ito S, Itou T, Yasumura M, Yoshinaka Y, et al. Mechanism of lipid-lowering action of the dipeptidyl peptidase-4 inhibitor, anagliptin, in low-density lipoprotein receptor-deficient mice. J Diabetes Investig. 2017;8(2):155–60. https://doi.org/10.1111/jdi.12593.
Rufinatscha K, Radlinger B, Dobner J, Folie S, Bon C, Profanter E, et al. Dipeptidyl peptidase-4 impairs insulin signaling and promotes lipid accumulation in hepatocytes. Biochem Biophys Res Commun. 2017;485(2):366–71. https://doi.org/10.1016/j.bbrc.2017.02.071.
Mostafa AM, Hamdy NM, Abdel-Rahman SZ, El-Mesallamy HO. Effect of vildagliptin and pravastatin combination on cholesterol efflux in adipocytes. IUBMB Life. 2016:535–43. https://doi.org/10.1002/iub.1510.
Renna NF, Diez EA, Miatello RM. Effects of dipeptidyl-peptidase 4 inhibitor about vascular inflammation in a metabolic syndrome model. PloS one. 2014;9(9):e106563-e. https://doi.org/10.1371/journal.pone.0106563.
Briand F, Thieblemont Q, Burcelin R, Sulpice T. Sitagliptin promotes macrophage-to-faeces reverse cholesterol transport through reduced intestinal cholesterol absorption in obese insulin resistant CETP-apoB100 transgenic mice. Diabetes Obes Metab. 2012;14(7):662–5. https://doi.org/10.1111/j.1463-1326.2012.01568.x.
Xu B, Shen T, Chen L, Xia J, Zhang C, Wang H, et al. The effect of sitagliptin on lipid metabolism of fatty liver mice and related mechanisms. Med Sci Monit. 2017;23:1363–70. https://doi.org/10.12659/MSM.900033.
Aroor AR, Habibi J, Ford DA, Nistala R, Lastra G, Manrique C, et al. Dipeptidyl peptidase-4 inhibition ameliorates western diet-induced hepatic steatosis and insulin resistance through hepatic lipid remodeling and modulation of hepatic mitochondrial function. Diabetes. 2015;64(6):1988–2001. https://doi.org/10.2337/db14-0804.
Liu H, Li N, Liu Y, Xing J, Feng S, Li M, et al. The dipeptidyl peptidase-4 inhibitor teneligliptin reduces kidney damage from hypercholesterolemia in apolipoprotein E-deficient mice. RSC Adv. 2017;7(14):8702–8. https://doi.org/10.1039/c6ra26718a.
Choi SH, Leem J, Park S, Lee CK, Park KG, Lee IK. Gemigliptin ameliorates western-diet-induced metabolic syndrome in mice. Can J Physiol Pharmacol. 2017;95(2):129–39. https://doi.org/10.1139/cjpp-2015-0026.
Zeng Y, Li C, Guan M, Zheng Z, Li J, Xu W, et al. The DPP-4 inhibitor sitagliptin attenuates the progress of atherosclerosis in apolipoprotein-E-knockout mice via AMPK- and MAPK-dependent mechanisms. Cardiovasc Diabetol. 2014;13(1). https://doi.org/10.1186/1475-2840-13-32.
Hirano T, Yamashita S, Takahashi M, Hashimoto H, Mori Y, Goto M. Anagliptin, a dipeptidyl peptidase-4 inhibitor, decreases macrophage infiltration and suppresses atherosclerosis in aortic and coronary arteries in cholesterol-fed rabbits. Metabolism. 2016;65(6):893–903. https://doi.org/10.1016/j.metabol.2016.03.010.
Brenner C, Franz WM, Kühlenthal S, Kuschnerus K, Remm F, Gross L, et al. DPP-4 inhibition ameliorates atherosclerosis by priming monocytes into M2 macrophages. Int J Cardiol. 2015;199:163–9. https://doi.org/10.1016/j.ijcard.2015.07.044.
Shah Z, Pineda C, Kampfrath T, Maiseyeu A, Ying Z, Racoma I, et al. Acute DPP-4 inhibition modulates vascular tone through GLP-1 independent pathways. Vasc Pharmacol. 2011;55(1–3):2–9. https://doi.org/10.1016/j.vph.2011.03.001.
Liu L, Liu J, Wong WT, Tian XY, Lau CW, Wang YX, et al. Dipeptidyl peptidase 4 inhibitor sitagliptin protects endothelial function in hypertension through a glucagon-like peptide 1-dependent mechanism. Hypertension. 2012;60(3):833–41. https://doi.org/10.1161/HYPERTENSIONAHA.112.195115.
Hamidi Shishavan M, Henning RH, Van Buiten A, Goris M, Deelman LE, Buikema H. Metformin improves endothelial function and reduces blood pressure in diabetic spontaneously hypertensive rats independent from glycemia control: comparison to vildagliptin. Sci Rep. 2017;7(1). https://doi.org/10.1038/s41598-017-11430-7.
Koibuchi N, Hasegawa Y, Katayama T, Toyama K, Uekawa K, Sueta D, et al. DPP-4 inhibitor linagliptin ameliorates cardiovascular injury in salt-sensitive hypertensive rats independently of blood glucose and blood pressure. Cardiovasc Diabetol. 2014;13(1). https://doi.org/10.1186/s12933-014-0157-0.
Nakagami H, Pang Z, Shimosato T, Moritani T, Kurinami H, Koriyama H, et al. The dipeptidyl peptidase-4 inhibitor teneligliptin improved endothelial dysfunction and insulin resistance in the SHR/NDmcr-cp rat model of metabolic syndrome. Hypertens Res. 2014;37(7):629–35. https://doi.org/10.1038/hr.2014.53.
Reis F, Ferreira L, Teixeira-De-Lemos E, Pinto F, Parada B, Mega C, et al. Effects of sitagliptin treatment on dysmetabolism, inflammation, and oxidative stress in an animal model of type 2 diabetes (ZDF rat). Mediat Inflamm. 2010;2010:1–11. https://doi.org/10.1155/2010/592760.
Chen B, Moore A, Escobedo LV, Koletsky MS, Hou D, Koletsky RJ, et al. Sitagliptin lowers glucagon and improves glucose tolerance in prediabetic obese SHROB rats. Exp Biol Med (Maywood, NJ). 2011;236(3):309–14. https://doi.org/10.1258/ebm.2010.010161.
Takeda Y, Fujita Y, Honjo J, Yanagimachi T, Sakagami H, Takiyama Y, et al. Reduction of both beta cell death and alpha cell proliferation by dipeptidyl peptidase-4 inhibition in a streptozotocin-induced model of diabetes in mice. Diabetologia. 2012;55(2):404–12. https://doi.org/10.1007/s00125-011-2365-4.
Zhang X, Wang Z, Huang Y, Wang J. Effects of chronic administration of alogliptin on the development of diabetes and β-cell function in high fat diet/streptozotocin diabetic mice. Diabetes Obes Metab. 2011;13(4):337–47. https://doi.org/10.1111/j.1463-1326.2010.01354.x.
Turcot V, Bouchard L, Faucher G, Tchernof A, Deshaies Y, Pérusse L, et al. DPP4 gene DNA methylation in the omentum is associated with its gene expression and plasma lipid profile in severe obesity. Obesity. 2011;19(2):388–95. https://doi.org/10.1038/oby.2010.198.
Monami M, Vitale V, Ambrosio ML, Bartoli N, Toffanello G, Ragghianti B, et al. Effects on lipid profile of dipeptidyl peptidase 4 inhibitors, pioglitazone, acarbose, and sulfonylureas: meta-analysis of placebo-controlled trials. Adv Ther. 2012;29(9):736–46. https://doi.org/10.1007/s12325-012-0045-5.
Homma K, Yoshizawa J, Shiina Y, Ozawa H, Igarashi M, Matsuoka T, et al. A dipeptidyl Peptidase-4 inhibitor, teneligliptin, decreases plasma triglyceride-rich lipoprotein remnants in diabetic patients with chronic kidney disease undergoing hemodialysis. Drugs in R and D. 2017;17(3):397–402. https://doi.org/10.1007/s40268-017-0189-5.
Tahara N, Yamagishi SI, Bekki M, Kodama N, Nakamura T, Sugiyama Y, et al. Anagliptin, a dipeptidyl peptidase-4 inhibitor ameliorates arterial stiffness in association with reduction of remnant-like particle cholesterol and alanine transaminase levels in type 2 diabetic patients. Curr Vasc Pharmacol. 2016;14(6):552–62. https://doi.org/10.2174/1570161114666160625090212.
Ahn CH, Kim EK, Min SH, Oh TJ, Cho YM. Effects of gemigliptin, a dipeptidyl peptidase-4 inhibitor, on lipid metabolism and endotoxemia after a high-fat meal in patients with type 2 diabetes. Diabetes Obes Metab. 2017;19(3):457–62. https://doi.org/10.1111/dom.12831.
Fan M, Li Y, Zhang S. Effects of sitagliptin on lipid profiles in patients with type 2 diabetes mellitus: A meta-analysis of randomized clinical trials. Medicine (United States). 2016;95(2). https://doi.org/10.1097/MD.0000000000002386.
Tremblay AJ, Lamarche B, Kelly I, Charest A, Lépine MC, Droit A, et al. Effect of sitagliptin therapy on triglyceride-rich lipoprotein kinetics in patients with type 2 diabetes. Diabetes Obes Metab. 2014;16(12):1223–9. https://doi.org/10.1111/dom.12359.
Tsurutani Y, Omura M, Matsuzawa Y, Saito J, Higa M, Taniyama M, et al. Efficacy and safety of the dipeptidyl Peptidase-4 inhibitor Sitagliptin on atherosclerosis, β-cell function, and glycemic control in Japanese patients with type 2 diabetes mellitus who are treatment Naïve or poorly responsive to Antidiabetes agents: a multicenter, prospective observational, uncontrolled study. Curr Ther Res Clin Exp. 2017;84:26–31. https://doi.org/10.1016/j.curtheres.2016.12.002.
Duvnjak L, Blaslov K. Dipeptidyl peptidase-4 inhibitors improve arterial stiffness, blood pressure, lipid profile and inflammation parameters in patients with type 2 diabetes mellitus. Diabetol Metab Syndr. 2016;8(1). https://doi.org/10.1186/s13098-016-0144-6.
Evans M, Schweizer A, Foley JE. Blood pressure and fasting lipid changes after 24 weeks’ treatment with vildagliptin: a pooled analysis in >2,000 previously drug-naïve patients with type 2 diabetes mellitus. Vasc Health Risk Manag. 2016;12:337–40. https://doi.org/10.2147/VHRM.S112148.
Kusunoki M, Sato D, Nakamura T, Oshida Y, Tsutsui H, Natsume Y, et al. The beneficial effects of the DPP-4 inhibitor Alogliptin on hemoglobin A1c and serum lipids in Japanese patients with type 2 diabetes. Drug Res. 2015;66(1):18–22. https://doi.org/10.1055/s-0035-1547254.
Kakuda H, Kobayashi J, Kakuda M, Yamakawa J, Takekoshi N. The effect of anagliptin treatment on glucose metabolism and lipid metabolism, and oxidative stress in fasting and postprandial states using a test meal in Japanese men with type 2 diabetes. Endocrine. 2015;48(3):1005–9. https://doi.org/10.1007/s12020-014-0376-x.
Sakura H, Hashimoto N, Sasamoto K, Ohashi H, Hasumi S, Ujihara N, et al. Effect of sitagliptin on blood glucose control in patients with type 2 diabetes mellitus who are treatment naive or poorly responsive to existing antidiabetic drugs: The JAMP study. BMC Endocr Disord. 2016;16(1). https://doi.org/10.1186/s12902-016-0149-z.
Amber CF, Zeynep TK, Evren O, Yusuf B, Can AK, Belma T. Di-peptidyl peptidase-4 inhibitor sitagliptin protects vascular function in metabolic syndrome: possible role of epigenetic regulation. Mol Biol Rep. 2014;41(8):4853–63. https://doi.org/10.1007/s11033-014-3392-2.
Liu L, Liu J, Tian XY, Wong WT, Lau CW, Xu A, et al. Uncoupling protein-2 mediates DPP-4 inhibitor-induced restoration of endothelial function in hypertension through reducing oxidative stress. Antioxid Redox Signal. 2014;21(11):1571–81. https://doi.org/10.1089/ars.2013.5519.
Devin JK, Pretorius M, Nian H, Yu C, Billings FT, Brown NJ. Dipeptidyl-peptidase 4 inhibition and the vascular effects of glucagon-like peptide-1 and brain natriuretic peptide in the human forearm. J Am Heart Assoc. 2014;3(4). https://doi.org/10.1161/jaha.114.001075.
Wilson JR, Brown NJ, Nian H, Yu C, Bidlingmaier M, Devin JK. Dipeptidyl peptidase-4 inhibition potentiates stimulated growth hormone secretion and vasodilation in women. J Am Heart Assoc. 2018;7(5). https://doi.org/10.1161/jaha.117.008000.
Ogawa S, Ishiki M, Nako K, Okamura M, Senda M, Mori T, et al. Sitagliptin, a dipeptidyl peptidase-4 inhibitor, decreases systolic blood pressure in Japanese hypertensive patients with type 2 diabetes. Tohoku J Exp Med. 2011;223(2):133–5. https://doi.org/10.1620/tjem.223.133.
Kawasaki I, Hiura Y, Tamai A, Yoshida Y, Yakusiji Y, Ikuno Y, et al. Sitagliptin reduces the urine albumin-to-creatinine ratio in type 2 diabetes through decreasing both blood pressure and estimated glomerular filtration rate. J Diabetes. 2015;7(1):41–6. https://doi.org/10.1111/1753-0407.12153.
Cosenso-Martin LN, Giollo-Júnior LT, Martineli DD, Cesarino CB, Nakazone MA, Cipullo JP, et al. Twelve-week randomized study to compare the effect of vildagliptin vs. glibenclamide both added-on to metformin on endothelium function in patients with type 2 diabetes and hypertension. Diabetol Metab Syndr. 2015;7(1). https://doi.org/10.1186/s13098-015-0062-z.
Koren S, Shemesh-Bar L, Tirosh A, Peleg RK, Berman S, Hamad RA, et al. The effect of sitagliptin versus glibenclamide on arterial stiffness, blood pressure, lipids, and inflammation in type 2 diabetes mellitus patients. Diabetes Technol Ther. 2012;14(7):561–7. https://doi.org/10.1089/dia.2011.0296.
Widlansky ME, Puppala VK, Suboc TM, Malik M, Branum A, Signorelli K, et al. Impact of DPP-4 inhibition on acute and chronic endothelial function in humans with type 2 diabetes on background metformin therapy. Vasc Med (London, England). 2017;22(3):189–96. https://doi.org/10.1177/1358863x16681486.
Zhang X, Zhao Q. Effects of dipeptidyl peptidase-4 inhibitors on blood pressure in patients with type 2 diabetes: a systematic review and meta-analysis. J Hypertens. 2016;34(2):167–75. https://doi.org/10.1097/HJH.0000000000000782.
Jelsing J, Vrang N, van Witteloostuijn SB, Mark M, Klein T. The DPP4 inhibitor linagliptin delays the onset of diabetes and preserves beta-cell mass in non-obese diabetic mice. J Endocrinol. 2012;214(3):381–7. https://doi.org/10.1530/joe-11-0479.
Akarte AS, Srinivasan BP, Gandhi S. Vildagliptin selectively ameliorates GLP-1, GLUT4, SREBP-1c mRNA levels and stimulates beta-cell proliferation resulting in improved glucose homeostasis in rats with streptozotocin-induced diabetes. J Diabetes Complicat. 2012;26(4):266–74. https://doi.org/10.1016/j.jdiacomp.2012.03.013.
Otsuka Y, Yamaguchi S, Furukawa A, Kosuda M, Nakazaki M, Ishihara H. Addition of sitagliptin or metformin to insulin monotherapy improves blood glucose control via different effects on insulin and glucagon secretion in hyperglycemic Japanese patients with type 2 diabetes. Endocr J. 2015;62(2):133–43. https://doi.org/10.1507/endocrj.EJ14-0148.
Seck TL, Engel SS, Williams-Herman DE, Sisk CM, Golm GT, Wang H, et al. Sitagliptin more effectively achieves a composite endpoint for A1C reduction, lack of hypoglycemia and no body weight gain compared with glipizide. Diabetes Res Clin Pract. 2011;93(1):e15–e7. https://doi.org/10.1016/j.diabres.2011.03.006.
Krobot KJ, Ferrante SA, Davies MJ, Seck T, Meininger GE, Williams-Herman D, et al. Lower risk of hypoglycemia with sitagliptin compared to glipizide when either is added to metformin therapy: a pre-specified analysis adjusting for the most recently measured HbA1c value. Curr Med Res Opin. 2012;28(8):1281–7. https://doi.org/10.1185/03007995.2012.703134.
Vellanki P, Smiley DD, Stefanovski D, Anzola I, Duan W, Hudson M, et al. Randomized controlled study of metformin and Sitagliptin on Long-term Normoglycemia remission in African American patients with hyperglycemic crises. Diabetes Care. 2016;39(11):1948–55. https://doi.org/10.2337/dc16-0406.
Kusunoki Y, Katsuno T, Myojin M, Miyakoshi K, Ikawa T, Matsuo T, et al. Effect of additional administration of acarbose on blood glucose fluctuations and postprandial hyperglycemia in patients with type 2 diabetes mellitus under treatment with alogliptin. Endocr J. 2013;60(4):431–9.
Osonoi T, Saito M, Tamasawa A, Ishida H, Osonoi Y. Effects of sitagliptin or mitiglinide as an add-on to acarbose on daily blood glucose fluctuations measured by 72 h subcutaneous continuous glucose monitoring in Japanese patients with type 2 diabetes: a prospective randomized study. Expert Opin Pharmacother. 2014;15(10):1325–35. https://doi.org/10.1517/14656566.2014.920323.
Pasquel FJ, Gianchandani R, Rubin DJ, Dungan KM, Anzola I, Gomez PC, et al. Efficacy of sitagliptin for the hospital management of general medicine and surgery patients with type 2 diabetes (Sita-Hospital): a multicentre, prospective, open-label, non-inferiority randomised trial. Lancet Diabetes Endocrinol. 2017;5(2):125–33. https://doi.org/10.1016/s2213-8587(16)30402-8.
Dejager S, Schweizer A. Minimizing the risk of hypoglycemia with vildagliptin: clinical experience, mechanistic basis, and importance in type 2 diabetes management. Diabetes Ther. 2011;2(2):51–66. https://doi.org/10.1007/s13300-010-0018-0.
Ahrén B, Foley JE, Dejager S, Akacha M, Shao Q, Heimann G, et al. Higher risk of hypoglycemia with glimepiride versus Vildagliptin in patients with type 2 diabetes is not driven by high doses of glimepiride: divergent patient susceptibilities? Diabetes Ther. 2014;5(2):459–69. https://doi.org/10.1007/s13300-014-0082-y.
Yang W, Xing X, Lv X, Li Y, Ma J, Yuan G, et al. Vildagliptin added to sulfonylurea improves glycemic control without hypoglycemia and weight gain in Chinese patients with type 2 diabetes mellitus. J Diabetes. 2015;7(2):174–81. https://doi.org/10.1111/1753-0407.12169.
Ning G, Wang W, Li L, Ma J, Lv X, Yang M, et al. Vildagliptin as add-on therapy to insulin improves glycemic control without increasing risk of hypoglycemia in Asian, predominantly Chinese, patients with type 2 diabetes mellitus. J Diabetes. 2016;8(3):345–53. https://doi.org/10.1111/1753-0407.12303.
Qiu Y, Luan X, Chen J, Kong Y, Xu X. Effects of vildagliptin on blood glucose fluctuation in patients with end-stage renal disease under hemodialysis in type 2 diabetes mellitus. Int J Clin Exp Med. 2016;9(6):9557–62.
Aravind SR, Ismail SB, Balamurugan R, Gupta JB, Wadhwa T, Loh SM, et al. Hypoglycemia in patients with type 2 diabetes from India and Malaysia treated with sitagliptin or a sulfonylurea during Ramadan: a randomized, pragmatic study. Curr Med Res Opin. 2012;28(8):1289–96. https://doi.org/10.1185/03007995.2012.707119.
Mbanya JC, Al-Sifri S, Abdel-Rahim A, Satman I. Incidence of hypoglycemia in patients with type 2 diabetes treated with gliclazide versus DPP-4 inhibitors during Ramadan: a meta-analytical approach. Diabetes Res Clin Pract. 2015;109(2):226–32. https://doi.org/10.1016/j.diabres.2015.04.030.
Raju A, Shetty S, Cai B, D'Souza AO. Hypoglycemia incidence rates and associated health care costs in patients with type 2 diabetes mellitus treated with second-line linagliptin or sulfonylurea after metformin monotherapy. J Manag Care Spec Pharm. 2016;22(5):483–92. https://doi.org/10.18553/jmcp.2016.22.5.483.
Eto T, Inoue S, Kadowaki T. Effects of once-daily teneligliptin on 24-h blood glucose control and safety in Japanese patients with type 2 diabetes mellitus: a 4-week, randomized, double-blind, placebo-controlled trial. Diabetes Obes Metab. 2012;14(11):1040–6. https://doi.org/10.1111/j.1463-1326.2012.01662.x.
Sicras-Mainar A, Navarro-Artieda R. Healthcare costs of the combination of metformin/dipeptidyl peptidase-4 inhibitors compared with metformin/other oral antidiabetes agents in patients with type 2 diabetes and metabolic syndrome. Diabetes Technol Ther. 2014;16(11):722–7. https://doi.org/10.1089/dia.2014.0091.
Underland LJ, Ilkowitz JT, Katikaneni R, Dowd A, Heptulla RA. Use of Sitagliptin with closed-loop technology to decrease postprandial blood glucose in type 1 diabetes. J Diabetes Sci Technol. 2017;11(3):602–10. https://doi.org/10.1177/1932296817699847.
Best C, Struthers H, Laciny E, Royal M, Reeds DN, Yarasheski KE. Sitagliptin reduces inflammation and chronic immune cell activation in HIV+ adults with impaired glucose tolerance. J Clin Endocrinol Metab. 2015;100(7):2621–9. https://doi.org/10.1210/jc.2015-1531.
van Genugten RE, van Raalte DH, Muskiet MH, Heymans MW, Pouwels PJ, Ouwens DM, et al. Does dipeptidyl peptidase-4 inhibition prevent the diabetogenic effects of glucocorticoids in men with the metabolic syndrome? A randomized controlled trial. Eur J Endocrinol. 2014;170(3):429–39. https://doi.org/10.1530/eje-13-0610.
Fadini GP, de Kreutzenberg SV, Gjini R, Avogaro A. The metabolic syndrome influences the response to incretin-based therapies. Acta Diabetol. 2011;48(3):219–25. https://doi.org/10.1007/s00592-011-0296-7.
Acknowledgements
The authors thank the Vice Chancellor of the Mashhad University of Medical Sciences, Mashhad, Iran.
Contribution
MR and BMR collected data and drafted the manuscript. HH gave the idea, designed and supervised the study. HH and GAF edited the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rameshrad, M., Razavi, B.M., Ferns, G.A.A. et al. Pharmacology of dipeptidyl peptidase-4 inhibitors and its use in the management of metabolic syndrome: a comprehensive review on drug repositioning. DARU J Pharm Sci 27, 341–360 (2019). https://doi.org/10.1007/s40199-019-00238-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40199-019-00238-7