Abstract
Background
The usefulness of dabigatran etexilate for the prevention of stroke in patients with atrial fibrillation (AF) has been reported.
Objectives
In this study the efficacy and safety of dabigatran etexilate for anticoagulation for AF ablation were examined.
Method
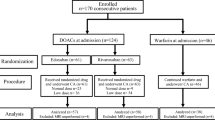
Patients were divided into three groups: Group 1, interrupted warfarin bridged by heparin between pre- and post-ablation; Group 2, continuous warfarin therapy; and Group 3, dabigatran etexilate therapy. Anticoagulation therapy with warfarin or dabigatran etexilate was performed from 30 days before to at least 90 days after AF ablation. Dabigatran etexilate was administered at 110 or 150 mg twice daily, depending on renal function and age.
Results
Patients’ clinical characteristics, associated disorders, echocardiographic parameters and arrhythmia status were not different among the three groups. Procedural parameters such as procedural time and radiofrequency energy supply were also not different among the three groups. The dabigatran etexilate group and the warfarin groups had no embolic complications (stroke, cerebral transient ischaemic attack, deep venous thrombosis or pulmonary embolism). No pericardial tamponade was observed in the dabigatran etexilate group, while two patients in each of Group 1 (2/194, 1.0 %) and Group 2 (2/203, 0.98 %) developed cardiac tamponade, though the differences were not significant. Pericardial effusion and groin haematoma were observed in one patient each (1/105, 0.9 %) in the dabigatran etexilate group, and the incidences were not different from the warfarin group (Group 1: 4/194, 2.1 % and 2/194, 1.0 %; Group 2: 3/203, 1.5 % and 2/203, 1.0 %, respectively). As a whole, the safety outcomes did not differ among the three groups.
Conclusion
Dabigatran etexilate is an effective and safe anticoagulation therapy for AF ablation. Thus, dabigatran etexilate appears to be useful as an alternative anticoagulant therapy to warfarin for AF ablation.

Similar content being viewed by others
References
Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25.
Benjamin EJ, Wolf PA, D’Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–52.
Seshadri N, Marrouche NF, Wilber D, et al. Pulmonary vein isolation for treatment of atrial fibrillation: recent updates. Pacing Clin Electrophysiol. 2003;26:1636–40.
Berkowitsch A, Greiss H, Vukajlovic D, et al. Usefulness of atrial fibrillation burden as a predictor for success of pulmonary vein isolation. Pacing Clin Electrophysiol. 2005;28:1292–301.
Macle L, Jais P, Weerasooriya R, et al. Irrigated-tip catheter ablation of pulmonary veins for treatment of atrial fibrillation. J Cardiovasc Electrophysiol. 2002;13:1067–73.
Kumagai K, Noguchi H, Ogawa M, et al. New approach to pulmonary vein isolation for atrial fibrillation using a multielectrode basket catheter. Circ J. 2006;70:88–93.
Yamane T, Date T, Kanzaki Y, et al. Segmental pulmonary vein antrum isolation using the “large-size” lasso catheter in patients with atrial fibrillation. Circ J. 2007;71:753–60.
Calkins H, Brugada J, Packer DL, et al. HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation developed in partnership with the European Heart Rhythm Association (EHRA) and the European Cardiac Arrhythmia Society (ECAS); in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), and the Society of Thoracic Surgeons (STS). Endorsed and approved by the governing bodies of the American College of Cardiology, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, and the Heart Rhythm Society. Europace. 2007;9:335–79.
Cappato R, Calkins H, Chen SA, et al. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005;111:1100–5.
Dixit S, Marchlinski FE. How to recognize, manage, and prevent complications during atrial fibrillation ablation. Heart Rhythm. 2007;4:108–15.
Scherr D, Sharma K, Dalal D, et al. Incidence and predictors of periprocedural cerebrovascular accident in patients undergoing catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2009;20:1357–63.
Oral H, Chugh A, Ozaydin M, et al. Risk of thromboembolic events after percutaneous left atrial radiofrequency ablation of atrial fibrillation. Circulation. 2006;114:759–65.
Pappone C, Santinelli V. How to perform encircling ablation of the left atrium. Heart Rhythm. 2006;3:1105–9.
Ren JF, Marchlinski FE, Callans DJ, et al. Increased intensity of anticoagulation may reduce risk of thrombus during atrial fibrillation ablation procedures in patients with spontaneous echo contrast. J Cardiovasc Electrophysiol. 2005;16:474–7.
Santangeli P, Di Biase L, Sanchez JE, et al. Atrial fibrillation ablation without interruption of anticoagulation. Cardiol Res Pract. 2011;2011:837841.
Connolly SJ, Pogue J, Eikelboom J, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008;118:2029–37.
Wann LS, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on dabigatran): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2011;57:1330–7.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Lakkireddy D, Reddy YM, Di Biase L, et al. Feasibility and safety of dabigatran versus warfarin for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. J Am Coll Cardiol. 2012;59:1168–74.
Winkle RA, Mead RH, Engel G, et al. The use of dabigatran immediately after atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2012;23:264–8.
Kottkamp H, Hindricks G, Eitel C, et al. Deep sedation for catheter ablation of atrial fibrillation: a prospective study in 650 consecutive patients. J Cardiovasc Electrophysiol. 2011;22:1339–43.
Kaseno K, Naito S, Nakamura K, et al. Efficacy and safety of periprocedural dabigatran in patients undergoing catheter ablation of atrial fibrillation. Circ J. 2012;76:2337–42.
World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2000;284:3043–5.
Jais P, Cauchemez B, Macle L, et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation. 2008;118:2498–505.
Di Biase L, Elayi CS, Fahmy TS, et al. Atrial fibrillation ablation strategies for paroxysmal patients: randomized comparison between different techniques. Circ Arrhythm Electrophysiol. 2009;2:113–9.
Schmidt B, Tilz RR, Neven K, et al. Remote robotic navigation and electroanatomical mapping for ablation of atrial fibrillation: considerations for navigation and impact on procedural outcome. Circ Arrhythm Electrophysiol. 2009;2:120–8.
Rostock T, Steven D, Hoffmann B, et al. Chronic atrial fibrillation is a biatrial arrhythmia: data from catheter ablation of chronic atrial fibrillation aiming arrhythmia termination using a sequential ablation approach. Circ Arrhythm Electrophysiol. 2008;1:344–53.
Wazni OM, Beheiry S, Fahmy T, et al. Atrial fibrillation ablation in patients with therapeutic international normalized ratio: comparison of strategies of anticoagulation management in the periprocedural period. Circulation. 2007;116:2531–4.
Stangier J. Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate. Clin Pharmacokinet. 2008;47:285–95.
Sanford M, Plosker GL. Dabigatran etexilate. Drugs. 2008;68:1699–709.
Stangier J, Rathgen K, Stahle H, et al. The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol. 2007;64:292–303.
Walenga JM, Adiguzel C. Drug and dietary interactions of the new and emerging oral anticoagulants. Int J Clin Pract. 2010;64:956–67.
Prudente LA, Moorman JR, Lake D, et al. Femoral vascular complications following catheter ablation of atrial fibrillation. J Interv Card Electrophysiol. 2009;26:59–64.
Flaker G, Ezekowitz M, Yusuf S, et al. Efficacy and safety of dabigatran compared to warfarin in patients with paroxysmal, persistent, and permanent atrial fibrillation: results from the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) study. J Am Coll Cardiol. 2012;59:854–5.
Pink J, Lane S, Pirmohamed M, et al. Dabigatran etexilate versus warfarin in management of non-valvular atrial fibrillation in UK context: quantitative benefit-harm and economic analyses. BMJ. 2011;343:d6333.
Acknowledgments
The authors have no conflicts of interest that are relevant to the content of this article. No sources of funding were used to assist in the conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamaji, H., Murakami, T., Hina, K. et al. Usefulness of Dabigatran Etexilate as Periprocedural Anticoagulation Therapy for Atrial Fibrillation Ablation. Clin Drug Investig 33, 409–418 (2013). https://doi.org/10.1007/s40261-013-0081-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-013-0081-1