Key Points
-
Approximately 2% of patients who present to hospital with suspected acute coronary syndrome have Takotsubo syndrome, with a predominance in postmenopausal women
-
Mortality is higher than initially thought, and recurrence is seen in 1.2% of patients within 6 months and nearly 5% at 6 years, with no preventive therapy currently available
-
Systemic catecholamine surges can cause acute coronary and peripheral vasospasm followed by peripheral vasodilation; a common complication is cardiogenic shock, due at least in part to left ventricular systolic dysfunction
-
Biopsy samples taken during the acute phase of Takotsubo syndrome show morphological changes similar to those after catecholamine-induced cardiotoxic effects, supporting direct effects as well as vascular influences
-
The apical myocardium of the left ventricle has a high density of β-adrenoceptors and, therefore, is the region most sensitive to circulating catecholamines
-
During extreme stress, excessive epinephrine levels cause a switch from the Gsα stimulatory to the cardioprotective Giα cardioinhibitory secondary messenger pathway within cardiomyocytes, thereby acting as a positive inotrope
Abstract
Takotsubo syndrome is an acute cardiac syndrome first described in 1990 and characterized by transient left ventricular dysfunction affecting more than one coronary artery territory, often in a circumferential apical, mid-ventricular, or basal distribution. Several pathophysiological explanations have been proposed for this syndrome and its intriguing appearance, and awareness is growing that these explanations might not be mutually exclusive. The reversible apical myocardial dysfunction observed might result from more than one pathophysiological phenomenon. The pathophysiology of Takotsubo syndrome is complex and integrates neuroendocrine physiology, potentially involving the cognitive centres of the brain, and including the hypothalamic–pituitary–adrenal axis. Cardiovascular responses are caused by the sudden sympathetic activation and surge in concentrations of circulating catecholamines. The multiple morphological changes seen in the myocardium match those seen after catecholamine-induced cardiotoxicity. The acute prognosis and recurrence rate are now known to be worse than initially thought, and much still needs to be learned about the epidemiology and the underlying pathophysiology of this fascinating condition in order to improve diagnostic and treatment pathways.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
08 June 2015
In the version of this Review published online ahead of print, the details of the author contributions were missing. The author contributions are now included in the HTML and PDF versions of the article.
References
Dote, K., Sato, H., Tateishi, H., Uchida, T. & Ishihara, M. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases [Japanese]. J. Cardiol. 21, 203–214 (1991).
Chan, C. et al. Acute myocardial infarction and stress cardiomyopathy following the Christchurch earthquakes. PLoS ONE 8, e68504 (2013).
Maron, B. J. et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 113, 1807–1816 (2006).
Elliott, P. et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 29, 270–276 (2008).
Deshmukh, A. et al. Prevalence of Takotsubo cardiomyopathy in the United States. Am. Heart J. 164, 66–71 (2012).
Prasad, A., Lerman, A. & Rihal, C. S. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am. Heart J. 155, 408–417 (2008).
Kurowski, V. et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest 132, 809–816 (2007).
Akashi, Y. J., Goldstein, D. S., Barbaro, G. & Ueyama, T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation 118, 2754–2762 (2008).
Primetshofer, D., Agladze, R., Kratzer, H., Reisinger, J. & Siostrzonek, P. Tako-Tsubo syndrome: an important differential diagnosis in patients with acute chest pain. Wien. Klin. Wochenschr. 122, 37–44 (2010).
Patel, S. M., Chokka, R. G., Prasad, K. & Prasad, A. Distinctive clinical characteristics according to age and gender in apical ballooning syndrome (takotsubo/stress cardiomyopathy): an analysis focusing on men and young women. J. Card. Fail. 19, 306–310 (2013).
Murakami, T. et al. Characterization of predictors of in-hospital cardiac complications of takotsubo cardiomyopathy: multi-center registry from Tokyo CCU Network. J. Cardiol. 63, 269–273 (2014).
Isogai, T. et al. Out-of-hospital versus in-hospital Takotsubo cardiomyopathy: analysis of 3719 patients in the Diagnosis Procedure Combination database in Japan. Int. J. Cardiol. 176, 413–417 (2014).
Kawai, S., Kitabatake, A., Tomoike, H & Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ. J. 71, 990–992 (2007).
Omerovic, E. How to think about stress-induced cardiomyopathy?—Think “out of the box”! Scand. Cardiovasc. J. 45, 67–71 (2011).
Eitel, I. et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 306, 277–286 (2011).
Parodi, G. et al. Revised clinical diagnostic criteria for Tako-tsubo syndrome: the Tako-tsubo Italian Network proposal. Int. J. Cardiol. 172, 282–283 (2014).
Akashi, Y. J., Nef, H. M., Mollmann, H. & Ueyama, T. Stress cardiomyopathy. Annu. Rev. Med. 61, 271–286 (2010).
Dib, C. et al. Clinical correlates and prognostic significance of electrocardiographic abnormalities in apical ballooning syndrome (Takotsubo/stress-induced cardiomyopathy). Am. Heart J. 157, 933–938 (2009).
Kosuge, M. et al. Simple and accurate electrocardiographic criteria to differentiate takotsubo cardiomyopathy from anterior acute myocardial infarction. J. Am. Coll. Cardiol. 55, 2514–2516 (2010).
Tamura, A. et al. A new electrocardiographic criterion to differentiate between Takotsubo cardiomyopathy and anterior wall ST-segment elevation acute myocardial infarction. Am. J. Cardiol. 108, 630–633 (2011).
Takashio, S. et al. Usefulness of SUM of ST-segment elevation on electrocardiograms (limb leads) for predicting in-hospital complications in patients with stress (takotsubo) cardiomyopathy. Am. J. Cardiol. 109, 1651–1656 (2012).
Kosuge, M. & Kimura, K. Electrocardiographic findings of takotsubo cardiomyopathy as compared with those of anterior acute myocardial infarction. J. Electrocardiol. 47, 684–689 (2014).
Johnson, N. P., Chavez, J. F., Mosley, W. J. 2nd, Flaherty, J. D. & Fox, J. M. Performance of electrocardiographic criteria to differentiate Takotsubo cardiomyopathy from acute anterior ST elevation myocardial infarction. Int. J. Cardiol. 164, 345–348 (2013).
Otalvaro, L., Zambrano, J. P. & Fishman, J. E. Takotsubo cardiomyopathy: utility of cardiac computed tomography angiography for acute diagnosis. J. Thorac. Imaging 26, W83–85 (2011).
Ogura, R. et al. Specific findings of the standard 12-lead ECG in patients with 'Takotsubo' cardiomyopathy: comparison with the findings of acute anterior myocardial infarction. Circ. J. 67, 687–690 (2003).
Kurisu, S. et al. Time course of electrocardiographic changes in patients with tako-tsubo syndrome: comparison with acute myocardial infarction with minimal enzymatic release. Circ. J. 68, 77–81 (2004).
Mitsuma, W. et al. Serial electrocardiographic findings in women with Takotsubo cardiomyopathy. Am. J. Cardiol. 100, 106–109 (2007).
Jabara, R. et al. Comparison of the clinical characteristics of apical and non-apical variants of “broken heart” (takotsubo) syndrome in the United States. J. Invasive Cardiol. 21, 216–222 (2009).
Nishida, J. et al. “Ballooning” patterns in takotsubo cardiomyopathy reflect different clinical backgrounds and outcomes: a BOREAS-TCM study. Heart Vessels (in press).
Ueyama, T. et al. Estrogen attenuates the emotional stress-induced cardiac responses in the animal model of Tako-tsubo (Ampulla) cardiomyopathy. J. Cardiovasc. Pharmacol. 42 (Suppl. 1), S117–119 (2003).
Ueyama, T. et al. Chronic estrogen supplementation following ovariectomy improves the emotional stress-induced cardiovascular responses by indirect action on the nervous system and by direct action on the heart. Circ. J. 71, 565–573 (2007).
Elesber, A. A. et al. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J. Am. Coll. Cardiol. 50, 448–452 (2007).
Sharkey, S. W. et al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J. Am. Coll. Cardiol. 55, 333–341 (2010).
Schultz, T. et al. Stress-induced cardiomyopathy in Sweden: evidence for different ethnic predisposition and altered cardio-circulatory status. Cardiology 122, 180–186 (2012).
Song, B. G. et al. Clinical characteristics, ballooning pattern, and long-term prognosis of transient left ventricular ballooning syndrome. Heart Lung 39, 188–195 (2010).
Citro, R. et al. Differences in clinical features and in-hospital outcomes of older adults with tako-tsubo cardiomyopathy. J. Am. Geriatr. Soc. 60, 93–98 (2012).
Schneider, B. et al. Complications in the clinical course of tako-tsubo cardiomyopathy. Int. J. Cardiol. 176, 199–205 (2014).
Schneider, B. et al. Gender differences in the manifestation of tako-tsubo cardiomyopathy. Int. J. Cardiol. 166, 584–588 (2013).
Citro, R. et al. Echocardiographic correlates of acute heart failure, cardiogenic shock, and in-hospital mortality in tako-tsubo cardiomyopathy. JACC Cardiovasc. Imaging 7, 119–129 (2014).
Brinjikji, W., El-Sayed, A. M. & Salka, S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am. Heart J. 164, 215–221 (2012).
Singh, K. et al. Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy. Am. J. Cardiol. 113, 1420–1428 (2014).
Schneider, B., Athanasiadis, A. & Sechtem, U. Gender-related differences in takotsubo cardiomyopathy. Heart Fail. Clin. 9, 137–146 (2013).
Vriz, O. et al. Tako-tsubo cardiomyopathy: insights from a community hospital. J. Cardiovasc. Med. (Hagerstown) 14, 576–581 (2013).
Lee, P. H. et al. Outcomes of patients with stress-induced cardiomyopathy diagnosed by echocardiography in a tertiary referral hospital. J. Am. Soc. Echocardiogr. 23, 766–771 (2010).
Previtali, M. et al. Clinical characteristics and outcome of left ventricular ballooning syndrome in a European population. Am. J. Cardiol. 107, 120–125 (2011).
Shimizu, M. et al. J wave and fragmented QRS formation during the hyperacute phase in Takotsubo cardiomyopathy. Circ. J. 78, 943–949 (2014).
Singh, K. et al. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int. J. Cardiol. 174, 696–701 (2014).
Santoro, F. et al. Lack of efficacy of drug therapy in preventing takotsubo cardiomyopathy recurrence: a meta-analysis. Clin. Cardiol. 37, 434–439 (2014).
Nef, H. M. et al. Tako-Tsubo cardiomyopathy: intraindividual structural analysis in the acute phase and after functional recovery. Eur. Heart J. 28, 2456–2464 (2007).
Szardien, S. et al. Molecular basis of disturbed extracellular matrix homeostasis in stress cardiomyopathy. Int. J. Cardiol. 168, 1685–1688 (2013).
Nef, H. M. et al. Activated cell survival cascade protects cardiomyocytes from cell death in Tako-Tsubo cardiomyopathy. Eur. J. Heart Fail. 11, 758–764 (2009).
Randhawa, M. S., Dhillon, A. S., Taylor, H. C., Sun, Z. & Desai, M. Y. Diagnostic utility of cardiac biomarkers in discriminating Takotsubo cardiomyopathy from acute myocardial infarction. J. Card. Fail. 20, 2–8 (2014).
Nef, H. M. et al. Expression profiling of cardiac genes in Tako-Tsubo cardiomyopathy: insight into a new cardiac entity. J. Mol. Cell. Cardiol. 44, 395–404 (2008).
Nef, J. M. et al. Abnormalities in intracellular Ca2+ regulation contribute to the pathomechanism of Tako-Tsubo cardiomyopathy. Eur. Heart. J. 30, 2155–2164 (2009).
Nef, H. M. et al. Reduced sarcoplasmic reticulum Ca2+-ATPase activity and dephosphorylated phospholamban contribute to contractile dysfunction in human hibernating myocardium. Mol. Cell. Biochem. 282, 53–63 (2006).
Nef, H. M., Mollmann, H., Akashi, Y. J. & Hamm, C. W. Mechanisms of stress (Takotsubo) cardiomyopathy. Nat. Rev. Cardiol. 7, 187–193 (2010).
Lyon, A. R., Rees, P. S., Prasad, S., Poole-Wilson, P. A. & Harding, S. E. Stress (Takotsubo) cardiomyopathy-a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat. Clin. Pract. Cardiovasc. Med. 5, 22–29 (2008).
Wittstein, I. S. et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N. Engl. J. Med. 352, 539–548 (2005).
Wilkinson, D. J. et al. Sympathetic activity in patients with panic disorder at rest, under laboratory mental stress, and during panic attacks. Arch. Gen. Psychiatry 55, 511–520 (1998).
Jaguszewski, M. et al. A signature of circulating microRNAs differentiates takotsubo cardiomyopathy from acute myocardial infarction. Eur. Heart J. 35, 999–1006 (2014).
Baudry, A., Mouillet-Richard, S., Schneider, B., Launay, J. M. & Kellermann, O. miR-16 targets the serotonin transporter: a new facet for adaptive responses to antidepressants. Science 329, 1537–1541 (2010).
Bai, M. et al. Abnormal hippocampal BDNF and miR-16 expression is associated with depression-like behaviors induced by stress during early life. PLoS ONE 7, e46921 (2012).
Redfors, B. et al. Different catecholamines induce different patterns of takotsubo-like cardiac dysfunction in an apparently afterload dependent manner. Int. J. Cardiol. 174, 330–336 (2014).
Kurisu, S. et al. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am. Heart J. 143, 448–455 (2002).
Tsuchihashi, K. et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J. Am. Coll. Cardiol. 38, 11–18 (2001).
Patel, S. M., Lerman, A., Lennon, R. J. & Prasad, A. Impaired coronary microvascular reactivity in women with apical ballooning syndrome (Takotsubo/stress cardiomyopathy). Eur. Heart J. Acute Cardiovasc. Care 2, 147–152 (2013).
Pilgrim, T. M. & Wyss, T. R. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review. Int. J. Cardiol. 124, 283–292 (2008).
Angelini, P. Transient left ventricular apical ballooning: a unifying pathophysiologic theory at the edge of Prinzmetal angina. Catheter. Cardiovasc. Interv. 71, 342–352 (2008).
Abe, Y. et al. Assessment of clinical features in transient left ventricular apical ballooning. J. Am. Coll. Cardiol. 41, 737–742 (2003).
Stiermaier, T. et al. Frequency and significance of myocardial bridging and recurrent segment of the left anterior descending coronary artery in patients with takotsubo cardiomyopathy. Am. J. Cardiol. 114, 1204–1209 (2014).
Cocco, G. & Chu, D. Stress-induced cardiomyopathy: a review. Eur. J. Intern. Med. 18, 369–379 (2007).
Abraham, J. et al. Stress cardiomyopathy after intravenous administration of catecholamines and beta-receptor agonists. J. Am. Coll. Cardiol. 53, 1320–1325 (2009).
Shao, Y. et al. Novel rat model reveals important roles of beta-adrenoreceptors in stress-induced cardiomyopathy. Int. J. Cardiol. 168, 1943–1950 (2013).
Redfors, B. et al. Contrast echocardiography reveals apparently normal coronary perfusion in a rat model of stress-induced (Takotsubo) cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 15, 152–157 (2014).
Kawano, H., Okada, R. & Yano, K. Histological study on the distribution of autonomic nerves in the human heart. Heart Vessels 18, 32–39 (2003).
Mori, H. et al. Increased responsiveness of left ventricular apical myocardium to adrenergic stimuli. Cardiovasc. Res. 27, 192–198 (1993).
Brouri, F. et al. Blockade of beta 1- and desensitization of beta 2-adrenoceptors reduce isoprenaline-induced cardiac fibrosis. Eur. J. Pharmacol. 485, 227–234 (2004).
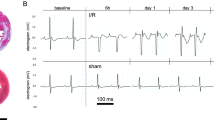
Paur, H. et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenergic receptor/Gi-dependent manner: a new model of takotsubo cardiomyopathy. Circulation 126, 697–706 (2012).
Heubach, J. F., Ravens, U. & Kaumann, A. J. Epinephrine activates both Gs and Gi pathways, but norepinephrine activates only the Gs pathway through human β2-adrenoceptors overexpressed in mouse heart. Mol. Pharmacol. 65, 1313–1322 (2004).
Heubach, J. F., Blaschke, M., Harding, S. E., Ravens, U. & Kaumann, A. J. Cardiostimulant and cardiodepressant effects through overexpressed human beta2-adrenoceptors in murine heart: regional differences and functional role of beta1-adrenoceptors. Naunyn Schmiedebergs Arch. Pharmacol. 367, 380–390 (2003).
Chesley, A. et al. The beta(2)-adrenergic receptor delivers an antiapoptotic signal to cardiac myocytes through G(i)-dependent coupling to phosphatidylinositol 3′-kinase. Circ. Res. 87, 1172–1179 (2000).
Land, S. et al. Computational modelling of Takotsubo cardiomyopathy: effect of spatially varying beta-adrenergic stimulation in the rat left ventricle. Am. J. Physiol. Heart Circ. Physiol. (2014).
Ieva, R. et al. Hyper-acute precipitating mechanism of Tako-Tsubo cardiomyopathy: in the beginning was basal hyperkinesis? Int. J. Cardiol. 167, e55–57 (2013).
Wright, P. T., Tranter, M. H., Morley-Smith, A. C. & Lyon, A. R. Pathophysiology of takotsubo syndrome: temporal phases of cardiovascular responses to extreme stress. Circ. J. 78, 1550–1558 (2014).
Sverrisdottir, Y. B., Schultz, T., Omerovic, E. & Elam, M. Sympathetic nerve activity in stress-induced cardiomyopathy. Clin. Auton. Res. 22, 259–264 (2012).
Redfors, B., Shao, Y., Ali, A. & Omerovic, E. Are the different patterns of stress-induced (Takotsubo) cardiomyopathy explained by regional mechanical overload and demand: supply mismatch in selected ventricular regions? Med. Hypotheses 81, 954–960 (2013).
Spinelli, L. et al. L41Q polymorphism of the G protein coupled receptor kinase 5 is associated with left ventricular apical ballooning syndrome. Eur. J. Heart Fail. 12, 13–16 (2010).
Liggett, S. B. et al. A GRK5 polymorphism that inhibits beta-adrenergic receptor signaling is protective in heart failure. Nat. Med. 14, 510–517 (2008).
Figtree, G. A. et al. No association of G-protein-coupled receptor kinase 5 or beta-adrenergic receptor polymorphisms with Takotsubo cardiomyopathy in a large Australian cohort. Eur. J. Heart Fail. 15, 730–733 (2013).
Kneale, B. J., Chowienczyk, P. J., Brett, S. E., Coltart, D. J. & Ritter, J. M. Gender differences in sensitivity to adrenergic agonists of forearm resistance vasculature. J. Am. Coll. Cardiol. 36, 1233–1238 (2000).
Patten, R. D. et al. 17beta-estradiol reduces cardiomyocyte apoptosis in vivo and in vitro via activation of phospho-inositide-3 kinase/Akt signaling. Circ. Res. 95, 692–699 (2004).
Ling, S., Komesaroff, P. & Sudhir, K. Cellular mechanisms underlying the cardiovascular actions of oestrogens. Clin. Sci. (Lond.) 111, 107–118 (2006).
Kam, K. W., Qi, J. S., Chen, M. & Wong, T. M. Estrogen reduces cardiac injury and expression of beta1-adrenoceptor upon ischemic insult in the rat heart. J. Pharmacol. Exp. Ther. 309, 8–15 (2004).
Desmet, W. J., Adriaenssens, B. F. & Dens, J. A. Apical ballooning of the left ventricle: first series in white patients. Heart 89, 1027–1031 (2003).
Bybee, K. A. et al. Clinical characteristics and thrombolysis in myocardial infarction frame counts in women with transient left ventricular apical ballooning syndrome. Am. J. Cardiol. 94, 343–346 (2004).
Akashi, Y. J. et al. Reversible ventricular dysfunction takotsubo cardiomyopathy. Eur. J. Heart Fail. 7, 1171–1176 (2005).
Sharkey, S. W. et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 111, 472–479 (2005).
Gianni, M. et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur. Heart J. 27, 1523–1529 (2006).
Hertting, K. et al. Transient left ventricular apical ballooning in a community hospital in Germany. Int. J. Cardiol. 112, 282–288 (2006).
Spedicato, L. et al. Transient left ventricular apical ballooning syndrome: a 4-year experience. J. Cardiovasc. Med. (Hagerstown) 9, 916–921 (2008).
El Mahmoud, R. et al. Prevalence and characteristics of left ventricular outflow tract obstruction in Tako-Tsubo syndrome. Am. Heart. J. 156, 543–548 (2008).
Previtali, M., Repetto, A., Panigada, S., Camporotondo, R. & Tavazzi, L. Left ventricular apical ballooning syndrome: prevalence, clinical characteristics and pathogenetic mechanisms in a European population. Int. J. Cardiol. 134, 91–96 (2009).
Eshtehardi, P. et al. Transient apical ballooning syndrome—clinical characteristics, ballooning pattern, and long-term follow-up in a Swiss population. Int. J. Cardiol. 135, 370–375 (2009).
Regnante, R. A. et al. Clinical characteristics and four-year outcomes of patients in the Rhode Island Takotsubo Cardiomyopathy Registry. Am. J. Cardiol. 103, 1015–1019 (2009).
Teh, A. W., New, G. & Cooke, J. A single-centre report on the characteristics of Tako-tsubo syndrome. Heart Lung Circ. 19, 63–70 (2010).
Parodi, G. et al. Natural history of tako-tsubo cardiomyopathy. Chest 139, 887–892 (2011).
Nunez-Gil, I. J. et al. Tako-tsubo syndrome and heart failure: long-term follow-up. Rev. Esp. Cardiol. (Engl. Ed.) 65, 996–1002 (2012).
Brenner, R. et al. Clinical characteristics, sex hormones, and long-term follow-up in swiss postmenopausal women presenting with takotsubo cardiomyopathy. Clin. Cardiol. 35, 340–347 (2012).
Samardhi, H. et al. Takotsubo cardiomyopathy: an Australian single centre experience with medium term follow up. Intern. Med. J. 42, 35–42 (2012).
Bellandi, B. et al. Epidemiology of Tako-tsubo cardiomyopathy: the Tuscany Registry for Tako-tsubo Cardiomyopathy [Italian]. G. Ital. Cardiol. (Rome) 13, 59–66 (2012).
Cacciotti, L. et al. Observational study on Takotsubo-like cardiomyopathy: clinical features, diagnosis, prognosis and follow-up. BMJ Open 2, e001165 (2012).
Sharma, V., Srinivasan, M., Sheehan, D. M. & Ionescu, A. Stress cardiomyopathy: case series and the review of literature. J. Emerg. Med. 45, e95–e98 (2013).
Pullara, A. et al. Takotsubo cardiomyopathy: real life management in the intensive coronary care unit. Minerva Med. 104, 537–544 (2013).
Showkathali, R. & Ramoutar, A. Takotsubo cardiomyopathy and acute coronary syndrome—overlapping diagnoses will lead to confusion. Eur. J. Intern. Med. 25, e78 (2014).
Acknowledgements
Y.J.A. is supported by the Grants-in-Aid for Scientific Research from Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Contributions
Y.J.A. researched data for the article. All authors substantially contributed to discussion of content, wrote, and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Akashi, Y., Nef, H. & Lyon, A. Epidemiology and pathophysiology of Takotsubo syndrome. Nat Rev Cardiol 12, 387–397 (2015). https://doi.org/10.1038/nrcardio.2015.39
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2015.39
This article is cited by
-
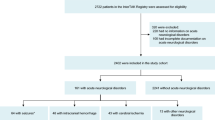
Development and validation of a prognostic nomogram for Takotsubo syndrome patients in the intensive care units: a retrospective cohort study
Scientific Reports (2023)
-
Takotsubo pathophysiology and complications: what we know and what we do not know
Heart Failure Reviews (2023)
-
Autonomic control of ventricular function in health and disease: current state of the art
Clinical Autonomic Research (2023)
-
Galectin-3-centered paracrine network mediates cardiac inflammation and fibrosis upon β-adrenergic insult
Science China Life Sciences (2023)
-
Takotsubo cardiomyopathy in a female presenting with status asthmaticus: a case report and review of literature
The Egyptian Heart Journal (2022)