-
PDF
- Split View
-
Views
-
Cite
Cite
Peter Eriksson, Lars Wilhelmsen, Annika Rosengren, Bundle-branch block in middle-aged men: risk of complications and death over 28 years: The Primary Prevention Study in Göteborg, Sweden, European Heart Journal, Volume 26, Issue 21, November 2005, Pages 2300–2306, https://doi.org/10.1093/eurheartj/ehi580
Close - Share Icon Share
Abstract
Aims To investigate the long-term fate of men with bundle-branch block (BBB) from a general population sample.
Methods and results Data were derived from 7392 men without a history of myocardial infarction or stroke, born between 1915 and 1925 and investigated between 1970 and 1973. All participants were followed from the date of their baseline examination until 1998. We identified 70 men with right-BBB and 46 men with left-BBB at baseline. In men with right-BBB, there was no increased risk of myocardial infarction, coronary death, heart failure, or all-cause mortality during follow-up. The multiple-adjusted hazard ratio for progression to high-degree atrioventricular block was 3.64 (99% confidence interval 0.79–16.72). In men with left-BBB, the hazard ratio for high-degree atrioventricular block was 12.89 (4.13–40.24). However, hazard ratio for all-cause mortality was 1.85 (1.15–2.97) when compared with men without BBB, mostly due to outside hospital coronary deaths, whose hazard ratio was 4.22 (1.90–9.34).
Conclusion The presence of BBB was strongly associated with future high-degree atrioventricular block that was more pronounced for left-BBB. Men with left-BBB have a substantially increased risk of coronary death, mainly due to sudden death outside the hospital setting.
See page 2222 for the editorial comment on this article (doi:10.1093/eurheartj/ehi390)
Introduction
Interest in bundle-branch block (BBB) has focussed primarily on its role as a predictor of mortality and co-existing cardiovascular disease. The epidemiological data have mostly been derived from hospitalized patients,1–8 with findings partly dependent on the characteristics of the patient cohort and the reason for carrying out an electrocardiogram (ECG). Studies performed in healthy populations have often had a wide age range with the majority of individuals with BBB found among the elderly.9–12 In a previous study, we found no correlation with risk factors for coronary heart disease, indicating that although ischaemic heart disease and BBB often co-exist, their causes may not be the same.13 Findings about future cardiovascular events have not been consistent,14,15 but several studies have found an increased mortality among patients with BBB and concomitant cardiovascular disease.1,3,8,16 In patients with acute myocardial infarction, the presence of BBB is a marker of worst outcome, which persists in the modern era of thrombolytic therapy.17–19 However, whether it is the pathogenesis and morphology of the BBB itself or the combination with ischaemic heart disease that has an impact on mortality is unclear. Although the annual incidence of progression to high-degree atrioventricular block has been reported to be 1–4% in unselected populations, bradyarrhythmias and high-degree atrioventricular block do not seem to have a major impact on mortality, and pacemaker treatment has not been found to diminish the risk of death in patients with BBB.3,20,21 Few studies have been able to investigate the long-term fate of individuals with BBB from a general population sample, with respect to ischaemic heart disease and other cardiovascular outcomes. In this study, we identified 70 men with right-BBB and 46 men with left-BBB in their 50s, followed them over a period of 28 years and compared them with 7276 men without BBB.***
Methods
Study population
The multifactor primary prevention trial started in Göteborg in 1970 and included all men in the city born between 1915 and 1925, except those born in 1923. A detailed account of the study rationale and design has been published.22 The intervention group of 10 000 men comprised a random third of the men in the trial, with two control groups of 10 000 men each. This study deals only with the men in the intervention group (n=9998), as only data from limited sub-samples were available for the control groups. In the intervention group, men who were found to be hypertensive, who had hypercholesterolaemia, or who smoked were referred to special intervention clinics. Ten years after entry, a 20% random sub-sample of the intervention group and one of the control groups were examined again. Serum cholesterol, smoking, and blood pressure had decreased in both groups, but there were no significant differences between the intervention and the control groups. In addition, there were no differences in outcome for cardiovascular, cancer, or all-cause mortality between the intervention and any of the control groups. The fact that the intervention was mainly targeted at subjects with very high risk and that changes in risk factors occurred among the general population as well contribute to explaining the lack of an overall effect of the intervention. So, we consider this study group to be reasonably representative of the background population in the city.
Data were derived from 7392 (out of a total of 7495) participating men, born between 1915 and 1925, except those born in 1923, without a history of prior myocardial infarction or stroke, and investigated between 1970 and 1973. All participants gave their written informed consent to participation in the study. The study was approved by the Ethics Committee for Medical Research at Göteborg University. Information on smoking habits, physical activity during leisure time, diabetes, myocardial infarction and stroke, symptoms of chest pain and dyspnoea on exertion, and family history of cardiovascular disease was collected via a mailed questionnaire to all men in the intervention group, including a Rose questionnaire for the presence of possible anginal symptoms and dyspnoea on exertion. Men who returned the questionnaire were invited to the study centre. Screening examinations recording weight, height, and blood pressure were performed in the afternoon, and samples for serum cholesterol concentration were taken after fasting for at least 2 h. Smoking habits were coded into five categories: never smoked, former smoker of more than 1 month's duration, smoking 1–14 g of tobacco per day, smoking 15–24 g, and smoking 25 g or more per day. One cigarette was considered to contain 1 g of tobacco, a cigarillo 2 g, and a cigar 5 g of tobacco. Physical activity during leisure time was categorized into three levels: (1) sedentary, (2) moderate activity, such as walking or light gardening for at least 4 h per week, and (3) regular, strenuous activity, or very strenuous activity. Possible anginal pain was defined as discomfort or pain in the chest provoked by walking two flights of stairs or on the level, relieved within 10 min by stopping or slowing down.
Electrocardiogram
Standard 12-lead ECGs were recorded, with the patient at rest in the supine position. Paper speed was 50 mm/s and calibration was 1 mV:10 mm. All 12-lead ECGs were interpreted by one of the authors (P.E.), who was blinded to all data, and were classified according to the presence or absence of BBB. Left-BBB was defined as (1) QRS duration >120 ms, (2) PQ interval >120 ms, (3) predominantly upright complexes with slurred R waves in lead I, V5, and V6, and (4) QS or rS pattern in V1. Right-BBB was defined as (1) QRS duration >120 ms, (2) PQ interval >120 ms, (3) rSR′ in lead V1 or V2, and (4) S waves in lead I and in either V5 or V6. Two men with left-BBB had concomitant atrial fibrillation and in those men the criterion of PQ interval >120 was waived.
Follow-up procedures
All participants in the multifactor Primary Prevention Study were followed from the date of their baseline examination until 31 December 1998, by running the data file of the men in the study against the Swedish national register on cause of death and the Swedish Hospital Discharge Register.23 This process was approved by the review board of the Göteborg University Ethics Committee. The Hospital Discharge Register has been in operation since 1964 and has operated on a nation-wide basis since 1987. However, all discharges from Sahlgrenska Hospital, which was the single major hospital in the city until 1977, have been entered in the national register since 1970 for all years (except 1976, due to a legislative change for that single year), and all discharges from Östra Hospital, the other major hospital in the city that opened in 1978, were entered from the start. In addition, until March 1983, all fatal and non-fatal myocardial infarctions occurring in the study population were recorded in the Göteborg AMI Register.24 End-points were defined as hospitalization or death according to the international classification of diseases (ICD) codes as in Table 1. Non-fatal myocardial infarction was defined as being hospitalized with acute myocardial infarction and surviving for at least 28 days. Out-of-hospital coronary death was defined as dying outside the hospital from coronary disease, at least 28 days after last being discharged from hospital. Pacemaker insertion was defined as operation codes 3081, 3082, 3083, 3094, 3097, or 3098. It should be noted that ICD 8 did not have a separate code for AV conduction defect III.
Statistical methods
We used the SAS statistical package (version 8e). For the cross-sectional analyses, Pearson's correlation tests were used for continuous variables and Mantel–Haenszel tests for categorical variables. All tests were two-sided and a P value of <0.05 was considered significant. In the prospective part of the study, age-adjusted proportional hazard analyses were used to calculate relative risks. Time at risk was calculated until 31 December 1998, death or hospitalization for any of the end-points. We used two final regression models, one with and one without the inclusion of covariates that may be intermediate factors in the causal chain between BBB and ischaemic heart disease. Thus, one regression model included only age, and two variables created from the two different types of BBB. The second model added systolic blood pressure, body mass index, serum cholesterol (entered as continuous variables), family history of myocardial infarction, treatment for hypertension, angina, diabetes, smoking, and leisure time physical activity. These variables were selected because they were significantly associated with AMI and coronary death in univariate analysis. We checked the assumption of proportional hazards by entering time-dependent variables related to the factors we studied. The impact of these variables was not significant on the model fit, which indicates that the assumption is valid. The linearity assumption was assessed by visual means. No adjustments were made to the significance levels to account for multiple testing; however, because we considered several outcomes, hazard ratios are presented with 99% confidence intervals.
Results
We identified 116 men with BBB (70 with right-BBB and 46 with left-BBB) at baseline. Men with BBB had higher mean blood pressure. There were no significant differences between men with (separately or combined) and without BBB for serum cholesterol, body mass index, smoking habits, leisure time physical activity, diabetes, or family history of myocardial infarction (Table 2).
Among men with right-BBB at baseline there was no increased risk of myocardial infarction or coronary death, atrial fibrillation, heart failure, and aortic stenosis or all-cause mortality during the 28 years of follow-up. However, the risk of developing high-degree atrioventricular block and/or to have a pacemaker inserted was increased approximately four times, compared with men without BBB (Table 3).
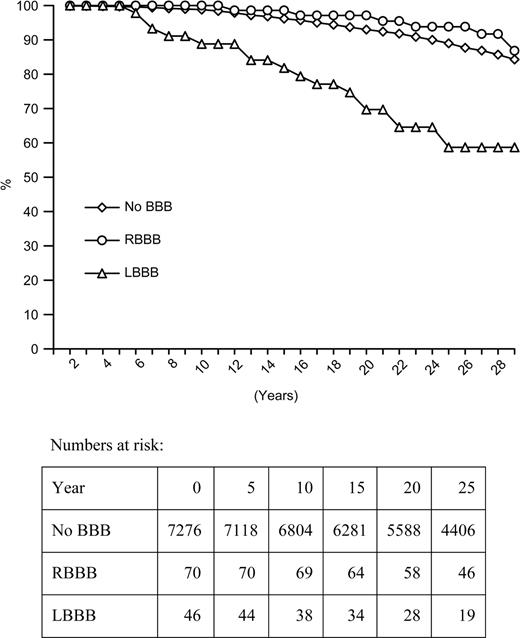
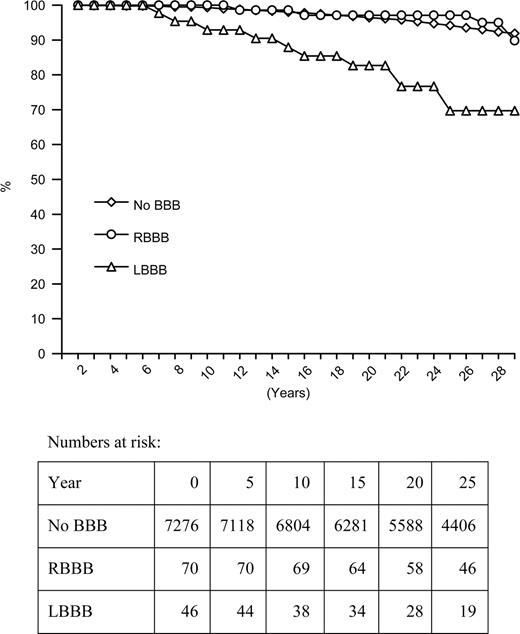
Men with left-BBB had an increased risk of myocardial infarction, mainly due to more fatal cases, particularly those occurring outside hospital, with a four-fold increase in risk that persisted after adjustment for systolic blood pressure and other risk factors. They had an 18-fold increased hazard of being diagnosed with high-degree atrioventricular block during follow-up and a 12-fold increased risk of requiring a pacemaker. Adjustment for blood pressure and other factors attenuated hazard ratios to some degree. Increased hazard of being hospitalized with heart failure or aortic stenosis was also observed (Table 3). The overall hazard of dying during follow-up was approximately twice that of the other men in the study. Survival curves for coronary deaths and sudden death are shown in Figures 1 and 2, respectively. An analysis restricted to men without possible angina pain or dyspnoea (5628 men without BBB, 60 with right-BBB, and 31 with left-BBB) did not decrease the hazard ratios associated with left-BBB (Table 4). However, the findings with respect to LBBB and aortic stenosis were no longer significant, largely because only three cases were diagnosed among men with LBBB [HR 3.77 (99% confidence interval 0.59–24.00)], and there was no significant association with all-cause mortality.
Discussion
Over almost 30 years of follow-up in this study we found that men with left, but not right, BBB had a markedly increased risk of dying from coronary disease and that two-thirds of these deaths occurred outside hospital, indicating probable fatal arrhythmia. One in six of the men with left-BBB progressed to high-degree atrioventricular block or to requiring a pacemaker. Men with right-BBB also progressed to high-degree atrioventricular block and/or to requiring a pacemaker to a greater extent than men without BBB, but otherwise did not have an increased risk of cardiovascular disease or death.
Classifying wide QRS complex as either right-BBB or left-BBB could be difficult, especially in the presence of ischaemia/acute myocardial infarction, when there is a risk of misinterpreting a peri-infarction block as BBB or a left-BBB as a sign of acute myocardial infarction. In our study, the ECG was taken routinely in a presumed healthy individual, in particular, excluding men with a history of acute myocardial infarction. Accordingly, we classified all participants with a QRS duration >120 ms as either right-BBB or left-BBB.
Several studies have tried to identify a relationship between the extent or location of coronary disease and the presence of BBB but have failed.16,25,26 Among patients with known coronary disease, no association was found between any particular location of coronary stenosis or left ventricular wall motion abnormalities, indicating that the BBB was not the result of an infarction in the area around the proximal conduction system. Except for elevated blood pressure, we found no association between any of the major risk factors and BBB, in accordance with an earlier study that found that coronary risk factors did not predict subsequent development of BBB.13 In this study, BBB was not significantly associated with future risk of non-fatal myocardial infarction, further supporting the hypothesis that coronary heart disease does probably not play a major role in the pathogenesis of BBB in a general male population.
The marked increase in mortality among patients with BBB observed in many studies is mainly seen in combination with concomitant cardiovascular disease, in particular, myocardial infarction.16,17,19,27–30 In BBB, the depolarization phase is by definition prolonged, usually more pronounced in left than in right-BBB. The prolongation of the vulnerable re-polarization phase, in combination with an increased number of premature ventricular beats secondary to ischaemic heart disease, might expose the individual to an increased risk of sudden ventricular tachyarrhythmias. An unexpectedly high prevalence of BBB was found in patients who survive ventricular fibrillation.31–33 This study supports the theory that individuals with left-BBB have a substantially increased risk of sudden death due to coronary causes, probably due to malignant tachyarrhythmias. The presence of BBB was strongly associated with future high-degree atrioventricular block that was more pronounced for left-BBB. This is in line with other studies that have shown a progression to high-degree atrioventricular block with an annual incidence of 1–4%.20,33,34 Bradyarrhythmias and high-degree atrioventricular block do not seem to have a major impact on mortality, and pacemaker treatment has not been found to diminish the risk of sudden death among individuals with BBB.14,20,21,35–37 For right-BBB, there was no increased risk of atrial fibrillation, heart failure, or aortic stenosis. In left-BBB, there was an increased risk of developing heart failure and aortic stenosis. We excluded men with known prior myocardial infarction or stroke, and men with BBB did not have more dyspnoea on exertion, but men with left-BBB had more possible anginal symptoms. Even so, an analysis that excluded men with these cardiovascular symptoms did not result in any change with respect to odds ratios, supporting the hypothesis that left-BBB is a marker for an adverse prognosis even in symptom-free men. Thus, BBB may be a marker of a slowly progressing disease that not only affects the conduction system.13
One of the limitations of this study was the fact that we had no information on subsequent development of BBB or of risk factors, i.e. diabetes or hypertension during the extended follow-up. In older individuals with more concomitant atherosclerosis, both the risk factor pattern and the outcome may be different. Also, we do not know to what extent a more detailed examination at baseline would have revealed other signs of heart disease. Owing to the small number of patients showing deviation of the frontal electrical axis, the contribution of this electrocardiographic pattern to the prognosis could not be determined. Another limitation is that we had no data on women. Meanwhile, the findings of this study indicate that a man in his 50s with right-BBB may be expected to have an increased risk of developing high-degree atrioventricular block but otherwise have normal longevity. Men with left-BBB have an even higher risk of developing high-degree atrioventricular block and more importantly have a substantially increased risk of coronary death, mainly due to sudden death outside the hospital setting.
Acknowledgement
This study was supported by grants from the Swedish Research Council and the Heart and Lung Foundation.
Conflict of interest: none declared
Figure 1 Survival curves for coronary deaths in men with left-BBB, right-BBB, and without BBB at baseline.
Figure 2 Survival curves for sudden deaths in men with left-BBB, right-BBB, and without BBB at baseline.
ICD codes used to define end-points
| . | ICDversiona . | ICDnumber . | |
|---|---|---|---|
| Myocardial infarction | 8–9 | 410 | |
| 10 | 121 | ||
| Coronary death | 8–9 | 410–414 | |
| 10 | I20–I25 | ||
| High-degree atrioventricular block (AV conduction defect II or III) | 8 | 427.20, 427.28 | |
| 9 | 426A | ||
| 10 | I44.2 | ||
| Atrial fibrillation | 8 | 427.92 | |
| 9 | 427D | ||
| 10 | I48 | ||
| Heart failure | 8 | 427.00, 427.10 | |
| 9 | 428A, 428B, 428X | ||
| 10 | I50 | ||
| Aortic stenosis | 8 | 395, 424.10, 424.11, 424.19 | |
| 9 | 395, 424B | ||
| 10 | I06, I35 |
| . | ICDversiona . | ICDnumber . | |
|---|---|---|---|
| Myocardial infarction | 8–9 | 410 | |
| 10 | 121 | ||
| Coronary death | 8–9 | 410–414 | |
| 10 | I20–I25 | ||
| High-degree atrioventricular block (AV conduction defect II or III) | 8 | 427.20, 427.28 | |
| 9 | 426A | ||
| 10 | I44.2 | ||
| Atrial fibrillation | 8 | 427.92 | |
| 9 | 427D | ||
| 10 | I48 | ||
| Heart failure | 8 | 427.00, 427.10 | |
| 9 | 428A, 428B, 428X | ||
| 10 | I50 | ||
| Aortic stenosis | 8 | 395, 424.10, 424.11, 424.19 | |
| 9 | 395, 424B | ||
| 10 | I06, I35 |
aICD 8 until 1986, ICD 9 until 1996, and ICD 10 from 1997.
ICD codes used to define end-points
| . | ICDversiona . | ICDnumber . | |
|---|---|---|---|
| Myocardial infarction | 8–9 | 410 | |
| 10 | 121 | ||
| Coronary death | 8–9 | 410–414 | |
| 10 | I20–I25 | ||
| High-degree atrioventricular block (AV conduction defect II or III) | 8 | 427.20, 427.28 | |
| 9 | 426A | ||
| 10 | I44.2 | ||
| Atrial fibrillation | 8 | 427.92 | |
| 9 | 427D | ||
| 10 | I48 | ||
| Heart failure | 8 | 427.00, 427.10 | |
| 9 | 428A, 428B, 428X | ||
| 10 | I50 | ||
| Aortic stenosis | 8 | 395, 424.10, 424.11, 424.19 | |
| 9 | 395, 424B | ||
| 10 | I06, I35 |
| . | ICDversiona . | ICDnumber . | |
|---|---|---|---|
| Myocardial infarction | 8–9 | 410 | |
| 10 | 121 | ||
| Coronary death | 8–9 | 410–414 | |
| 10 | I20–I25 | ||
| High-degree atrioventricular block (AV conduction defect II or III) | 8 | 427.20, 427.28 | |
| 9 | 426A | ||
| 10 | I44.2 | ||
| Atrial fibrillation | 8 | 427.92 | |
| 9 | 427D | ||
| 10 | I48 | ||
| Heart failure | 8 | 427.00, 427.10 | |
| 9 | 428A, 428B, 428X | ||
| 10 | I50 | ||
| Aortic stenosis | 8 | 395, 424.10, 424.11, 424.19 | |
| 9 | 395, 424B | ||
| 10 | I06, I35 |
aICD 8 until 1986, ICD 9 until 1996, and ICD 10 from 1997.
Coronary risk factors by the absence or presence of right- or left-bundle-branch block at baseline in 1970–1972
| . | No bundle-branch block (n=7276) . | RBBB (n=70) . | LBBB (n=46) . | Any bundle-branch block (n=116) . | P for comparisons with men without bundle-branch block . |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 51.6 (2.3) | 52.4 (2.0) | 52.1 (2.5) | 52.3 (2.2) | |
| SBP (mmHg), mean (SD) | 149 (22) | 154 (23) | 156 (25) | 155 (24) | RBBB 0.039; LBBB 0.025; any BBB 0.003 |
| DBP (mmHg), mean (SD) | 95 (13) | 97 (13) | 100 (16) | 98 (14) | LBBB 0.004; any BBB 0.006 |
| Serum cholesterol (mmol/l), mean (SD) | 6.46 (1.16) | 6.39 (1.11) | 6.57 (1.37) | 6.46 (1.16) | |
| Body mass index (kg * m−2), mean (SD) | 25.5 (3.3) | 25.8 (3.8) | 25.9 (2.8) | 25.9 (3.8) | |
| Smokers at baseline, % (n) | 50 (3647) | 50 (35) | 49 (22) | 50 (57) | |
| Sedentary physical activity, % (n) | 26 (1865) | 14 (10) | 30 (14) | 21 (24) | |
| Moderate activity, % (n) | 59 (4270) | 69 (48) | 59 (27) | 65 (75) | |
| Regular, strenuous activity or very strenuous activity, % (n) | 16 (1141) | 17 (12) | 11 (5) | 15 (17) | |
| Family history, % (n) | 20 (1448) | 17 (12) | 20 (9) | 18 (21) | |
| Diabetes, % (n) | 2 (143) | 1 (1) | 2 (1) | 2 (2) | |
| Treated hypertension, % (n) | 5 (387) | 6 (4) | 11 (5) | 8 (9) | |
| Presence of angina, % (n) | 6 (465) | 0 () | 17 (8) | 7 (8) | |
| Dyspnea walking 2 flights of stairs, % (n) | 20 (1473) | 14 (10) | 20 (9) | 16 (19) |
| . | No bundle-branch block (n=7276) . | RBBB (n=70) . | LBBB (n=46) . | Any bundle-branch block (n=116) . | P for comparisons with men without bundle-branch block . |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 51.6 (2.3) | 52.4 (2.0) | 52.1 (2.5) | 52.3 (2.2) | |
| SBP (mmHg), mean (SD) | 149 (22) | 154 (23) | 156 (25) | 155 (24) | RBBB 0.039; LBBB 0.025; any BBB 0.003 |
| DBP (mmHg), mean (SD) | 95 (13) | 97 (13) | 100 (16) | 98 (14) | LBBB 0.004; any BBB 0.006 |
| Serum cholesterol (mmol/l), mean (SD) | 6.46 (1.16) | 6.39 (1.11) | 6.57 (1.37) | 6.46 (1.16) | |
| Body mass index (kg * m−2), mean (SD) | 25.5 (3.3) | 25.8 (3.8) | 25.9 (2.8) | 25.9 (3.8) | |
| Smokers at baseline, % (n) | 50 (3647) | 50 (35) | 49 (22) | 50 (57) | |
| Sedentary physical activity, % (n) | 26 (1865) | 14 (10) | 30 (14) | 21 (24) | |
| Moderate activity, % (n) | 59 (4270) | 69 (48) | 59 (27) | 65 (75) | |
| Regular, strenuous activity or very strenuous activity, % (n) | 16 (1141) | 17 (12) | 11 (5) | 15 (17) | |
| Family history, % (n) | 20 (1448) | 17 (12) | 20 (9) | 18 (21) | |
| Diabetes, % (n) | 2 (143) | 1 (1) | 2 (1) | 2 (2) | |
| Treated hypertension, % (n) | 5 (387) | 6 (4) | 11 (5) | 8 (9) | |
| Presence of angina, % (n) | 6 (465) | 0 () | 17 (8) | 7 (8) | |
| Dyspnea walking 2 flights of stairs, % (n) | 20 (1473) | 14 (10) | 20 (9) | 16 (19) |
All comparisons are for the group without bundle-branch block.
Coronary risk factors by the absence or presence of right- or left-bundle-branch block at baseline in 1970–1972
| . | No bundle-branch block (n=7276) . | RBBB (n=70) . | LBBB (n=46) . | Any bundle-branch block (n=116) . | P for comparisons with men without bundle-branch block . |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 51.6 (2.3) | 52.4 (2.0) | 52.1 (2.5) | 52.3 (2.2) | |
| SBP (mmHg), mean (SD) | 149 (22) | 154 (23) | 156 (25) | 155 (24) | RBBB 0.039; LBBB 0.025; any BBB 0.003 |
| DBP (mmHg), mean (SD) | 95 (13) | 97 (13) | 100 (16) | 98 (14) | LBBB 0.004; any BBB 0.006 |
| Serum cholesterol (mmol/l), mean (SD) | 6.46 (1.16) | 6.39 (1.11) | 6.57 (1.37) | 6.46 (1.16) | |
| Body mass index (kg * m−2), mean (SD) | 25.5 (3.3) | 25.8 (3.8) | 25.9 (2.8) | 25.9 (3.8) | |
| Smokers at baseline, % (n) | 50 (3647) | 50 (35) | 49 (22) | 50 (57) | |
| Sedentary physical activity, % (n) | 26 (1865) | 14 (10) | 30 (14) | 21 (24) | |
| Moderate activity, % (n) | 59 (4270) | 69 (48) | 59 (27) | 65 (75) | |
| Regular, strenuous activity or very strenuous activity, % (n) | 16 (1141) | 17 (12) | 11 (5) | 15 (17) | |
| Family history, % (n) | 20 (1448) | 17 (12) | 20 (9) | 18 (21) | |
| Diabetes, % (n) | 2 (143) | 1 (1) | 2 (1) | 2 (2) | |
| Treated hypertension, % (n) | 5 (387) | 6 (4) | 11 (5) | 8 (9) | |
| Presence of angina, % (n) | 6 (465) | 0 () | 17 (8) | 7 (8) | |
| Dyspnea walking 2 flights of stairs, % (n) | 20 (1473) | 14 (10) | 20 (9) | 16 (19) |
| . | No bundle-branch block (n=7276) . | RBBB (n=70) . | LBBB (n=46) . | Any bundle-branch block (n=116) . | P for comparisons with men without bundle-branch block . |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 51.6 (2.3) | 52.4 (2.0) | 52.1 (2.5) | 52.3 (2.2) | |
| SBP (mmHg), mean (SD) | 149 (22) | 154 (23) | 156 (25) | 155 (24) | RBBB 0.039; LBBB 0.025; any BBB 0.003 |
| DBP (mmHg), mean (SD) | 95 (13) | 97 (13) | 100 (16) | 98 (14) | LBBB 0.004; any BBB 0.006 |
| Serum cholesterol (mmol/l), mean (SD) | 6.46 (1.16) | 6.39 (1.11) | 6.57 (1.37) | 6.46 (1.16) | |
| Body mass index (kg * m−2), mean (SD) | 25.5 (3.3) | 25.8 (3.8) | 25.9 (2.8) | 25.9 (3.8) | |
| Smokers at baseline, % (n) | 50 (3647) | 50 (35) | 49 (22) | 50 (57) | |
| Sedentary physical activity, % (n) | 26 (1865) | 14 (10) | 30 (14) | 21 (24) | |
| Moderate activity, % (n) | 59 (4270) | 69 (48) | 59 (27) | 65 (75) | |
| Regular, strenuous activity or very strenuous activity, % (n) | 16 (1141) | 17 (12) | 11 (5) | 15 (17) | |
| Family history, % (n) | 20 (1448) | 17 (12) | 20 (9) | 18 (21) | |
| Diabetes, % (n) | 2 (143) | 1 (1) | 2 (1) | 2 (2) | |
| Treated hypertension, % (n) | 5 (387) | 6 (4) | 11 (5) | 8 (9) | |
| Presence of angina, % (n) | 6 (465) | 0 () | 17 (8) | 7 (8) | |
| Dyspnea walking 2 flights of stairs, % (n) | 20 (1473) | 14 (10) | 20 (9) | 16 (19) |
All comparisons are for the group without bundle-branch block.
Cardiac end-points and hazard ratios by the absence or presence of right- or left-bundle-branch block at baseline in 1970–1972
| . | Number of cases . | Cases per 10 000 person years . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|---|
| Non-fatal myocardial infarction | ||||
| No bundle-branch block | 1046 | 62 | 1.00 | 1.00 |
| RBBB | 11 | 64 | 1.00 (0.46–2.18) | 1.11 (0.51–2.43) |
| LBBB | 10 | 110 | 1.78 (0.79–4.04) | 1.54 (0.68–3.49) |
| Acute myocardial infarction | ||||
| No bundle-branch block | 1654 | 103 | 1.00 | 1.00 |
| RBBB | 15 | 95 | 0.85 (0.43–1.65) | 0.94 (0.48–1.83) |
| LBBB | 22 | 256 | 2.58 (1.49–4.49) | 2.26 (1.29–3.94) |
| All coronary deaths | ||||
| No bundle-branch block | 891 | 52 | 1.00 | 1.00 |
| RBBB | 6 | 35 | 0.59 (0.20–1.69) | 0.65 (0.23–1.87) |
| LBBB | 17 | 186 | 3.75 (2.00–7.05) | 3.30 (1.75–6.24) |
| Out-of-hospital coronary deaths | ||||
| No bundle-branch block | 450 | 26 | 1.00 | 1.00 |
| RBBB | 4 | 23 | 0.78 (0.21–2.83) | 0.87 (0.24–3.18) |
| LBBB | 11 | 121 | 4.76 (2.17–10.46) | 4.22 (1.90–9.34) |
| High-degree atrioventricular block | ||||
| No bundle-branch block | 82 | 5 | 1.00 | 1.00 |
| RBBB | 3 | 18 | 3.15 (0.69–14.34) | 3.64 (0.79–16.72) |
| LBBB | 7 | 80 | 17.77 (6.42–49.20) | 12.89 (4.13–40.24) |
| Pacemaker | ||||
| No bundle-branch block | 144 | 8 | 1.00 | 1.00 |
| RBBB | 6 | 36 | 3.91 (1.33–11.45) | 4.45 (1.51–13.15) |
| LBBB | 7 | 81 | 11.73 (4.32–31.85) | 8.48 (2.85–25.30) |
| Atrial fibrillation | ||||
| No bundle-branch block | 873 | 53 | 1.00 | 1.00 |
| RBBB | 12 | 72 | 1.27 (0.60–2.68) | 1.33 (0.62–2.80) |
| LBBB | 9 | 105 | 2.39 (1.01–5.68) | 1.85 (0.74–4.63) |
| Heart failure | ||||
| No bundle-branch block | 1032 | 62 | 1.00 | 1.00 |
| RBBB | 14 | 84 | 1.22 (0.61–2.43) | 1.33 (0.66–2.66) |
| LBBB | 15 | 177 | 3.54 (1.81–6.92) | 3.26 (1.66–6.41) |
| Aortic stenosis | ||||
| No bundle-branch block | 178 | 10 | 1.00 | 1.00 |
| RBBB | 2 | 12 | 1.00 (0.16–6.29) | 1.10 (0.18–6.92) |
| LBBB | 5 | 58 | 5.98 (1.86–19.26) | 4.33 (1.16–16.13) |
| All-cause mortality | ||||
| No bundle-branch block | 3219 | 190 | 1.00 | 1.00 |
| RBBB | 29 | 169 | 0.80 (0.50–1.30) | 0.88 (0.54–1.42) |
| LBBB | 30 | 329 | 1.92 (1.20–3.08) | 1.85 (1.15–2.97) |
| . | Number of cases . | Cases per 10 000 person years . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|---|
| Non-fatal myocardial infarction | ||||
| No bundle-branch block | 1046 | 62 | 1.00 | 1.00 |
| RBBB | 11 | 64 | 1.00 (0.46–2.18) | 1.11 (0.51–2.43) |
| LBBB | 10 | 110 | 1.78 (0.79–4.04) | 1.54 (0.68–3.49) |
| Acute myocardial infarction | ||||
| No bundle-branch block | 1654 | 103 | 1.00 | 1.00 |
| RBBB | 15 | 95 | 0.85 (0.43–1.65) | 0.94 (0.48–1.83) |
| LBBB | 22 | 256 | 2.58 (1.49–4.49) | 2.26 (1.29–3.94) |
| All coronary deaths | ||||
| No bundle-branch block | 891 | 52 | 1.00 | 1.00 |
| RBBB | 6 | 35 | 0.59 (0.20–1.69) | 0.65 (0.23–1.87) |
| LBBB | 17 | 186 | 3.75 (2.00–7.05) | 3.30 (1.75–6.24) |
| Out-of-hospital coronary deaths | ||||
| No bundle-branch block | 450 | 26 | 1.00 | 1.00 |
| RBBB | 4 | 23 | 0.78 (0.21–2.83) | 0.87 (0.24–3.18) |
| LBBB | 11 | 121 | 4.76 (2.17–10.46) | 4.22 (1.90–9.34) |
| High-degree atrioventricular block | ||||
| No bundle-branch block | 82 | 5 | 1.00 | 1.00 |
| RBBB | 3 | 18 | 3.15 (0.69–14.34) | 3.64 (0.79–16.72) |
| LBBB | 7 | 80 | 17.77 (6.42–49.20) | 12.89 (4.13–40.24) |
| Pacemaker | ||||
| No bundle-branch block | 144 | 8 | 1.00 | 1.00 |
| RBBB | 6 | 36 | 3.91 (1.33–11.45) | 4.45 (1.51–13.15) |
| LBBB | 7 | 81 | 11.73 (4.32–31.85) | 8.48 (2.85–25.30) |
| Atrial fibrillation | ||||
| No bundle-branch block | 873 | 53 | 1.00 | 1.00 |
| RBBB | 12 | 72 | 1.27 (0.60–2.68) | 1.33 (0.62–2.80) |
| LBBB | 9 | 105 | 2.39 (1.01–5.68) | 1.85 (0.74–4.63) |
| Heart failure | ||||
| No bundle-branch block | 1032 | 62 | 1.00 | 1.00 |
| RBBB | 14 | 84 | 1.22 (0.61–2.43) | 1.33 (0.66–2.66) |
| LBBB | 15 | 177 | 3.54 (1.81–6.92) | 3.26 (1.66–6.41) |
| Aortic stenosis | ||||
| No bundle-branch block | 178 | 10 | 1.00 | 1.00 |
| RBBB | 2 | 12 | 1.00 (0.16–6.29) | 1.10 (0.18–6.92) |
| LBBB | 5 | 58 | 5.98 (1.86–19.26) | 4.33 (1.16–16.13) |
| All-cause mortality | ||||
| No bundle-branch block | 3219 | 190 | 1.00 | 1.00 |
| RBBB | 29 | 169 | 0.80 (0.50–1.30) | 0.88 (0.54–1.42) |
| LBBB | 30 | 329 | 1.92 (1.20–3.08) | 1.85 (1.15–2.97) |
aAdjustment for age, systolic blood pressure, serum cholesterol, body mass index, family history of myocardial infarction, treatment for hypertension, angina, diabetes, smoking, and leisure time physical activity.
Cardiac end-points and hazard ratios by the absence or presence of right- or left-bundle-branch block at baseline in 1970–1972
| . | Number of cases . | Cases per 10 000 person years . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|---|
| Non-fatal myocardial infarction | ||||
| No bundle-branch block | 1046 | 62 | 1.00 | 1.00 |
| RBBB | 11 | 64 | 1.00 (0.46–2.18) | 1.11 (0.51–2.43) |
| LBBB | 10 | 110 | 1.78 (0.79–4.04) | 1.54 (0.68–3.49) |
| Acute myocardial infarction | ||||
| No bundle-branch block | 1654 | 103 | 1.00 | 1.00 |
| RBBB | 15 | 95 | 0.85 (0.43–1.65) | 0.94 (0.48–1.83) |
| LBBB | 22 | 256 | 2.58 (1.49–4.49) | 2.26 (1.29–3.94) |
| All coronary deaths | ||||
| No bundle-branch block | 891 | 52 | 1.00 | 1.00 |
| RBBB | 6 | 35 | 0.59 (0.20–1.69) | 0.65 (0.23–1.87) |
| LBBB | 17 | 186 | 3.75 (2.00–7.05) | 3.30 (1.75–6.24) |
| Out-of-hospital coronary deaths | ||||
| No bundle-branch block | 450 | 26 | 1.00 | 1.00 |
| RBBB | 4 | 23 | 0.78 (0.21–2.83) | 0.87 (0.24–3.18) |
| LBBB | 11 | 121 | 4.76 (2.17–10.46) | 4.22 (1.90–9.34) |
| High-degree atrioventricular block | ||||
| No bundle-branch block | 82 | 5 | 1.00 | 1.00 |
| RBBB | 3 | 18 | 3.15 (0.69–14.34) | 3.64 (0.79–16.72) |
| LBBB | 7 | 80 | 17.77 (6.42–49.20) | 12.89 (4.13–40.24) |
| Pacemaker | ||||
| No bundle-branch block | 144 | 8 | 1.00 | 1.00 |
| RBBB | 6 | 36 | 3.91 (1.33–11.45) | 4.45 (1.51–13.15) |
| LBBB | 7 | 81 | 11.73 (4.32–31.85) | 8.48 (2.85–25.30) |
| Atrial fibrillation | ||||
| No bundle-branch block | 873 | 53 | 1.00 | 1.00 |
| RBBB | 12 | 72 | 1.27 (0.60–2.68) | 1.33 (0.62–2.80) |
| LBBB | 9 | 105 | 2.39 (1.01–5.68) | 1.85 (0.74–4.63) |
| Heart failure | ||||
| No bundle-branch block | 1032 | 62 | 1.00 | 1.00 |
| RBBB | 14 | 84 | 1.22 (0.61–2.43) | 1.33 (0.66–2.66) |
| LBBB | 15 | 177 | 3.54 (1.81–6.92) | 3.26 (1.66–6.41) |
| Aortic stenosis | ||||
| No bundle-branch block | 178 | 10 | 1.00 | 1.00 |
| RBBB | 2 | 12 | 1.00 (0.16–6.29) | 1.10 (0.18–6.92) |
| LBBB | 5 | 58 | 5.98 (1.86–19.26) | 4.33 (1.16–16.13) |
| All-cause mortality | ||||
| No bundle-branch block | 3219 | 190 | 1.00 | 1.00 |
| RBBB | 29 | 169 | 0.80 (0.50–1.30) | 0.88 (0.54–1.42) |
| LBBB | 30 | 329 | 1.92 (1.20–3.08) | 1.85 (1.15–2.97) |
| . | Number of cases . | Cases per 10 000 person years . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|---|
| Non-fatal myocardial infarction | ||||
| No bundle-branch block | 1046 | 62 | 1.00 | 1.00 |
| RBBB | 11 | 64 | 1.00 (0.46–2.18) | 1.11 (0.51–2.43) |
| LBBB | 10 | 110 | 1.78 (0.79–4.04) | 1.54 (0.68–3.49) |
| Acute myocardial infarction | ||||
| No bundle-branch block | 1654 | 103 | 1.00 | 1.00 |
| RBBB | 15 | 95 | 0.85 (0.43–1.65) | 0.94 (0.48–1.83) |
| LBBB | 22 | 256 | 2.58 (1.49–4.49) | 2.26 (1.29–3.94) |
| All coronary deaths | ||||
| No bundle-branch block | 891 | 52 | 1.00 | 1.00 |
| RBBB | 6 | 35 | 0.59 (0.20–1.69) | 0.65 (0.23–1.87) |
| LBBB | 17 | 186 | 3.75 (2.00–7.05) | 3.30 (1.75–6.24) |
| Out-of-hospital coronary deaths | ||||
| No bundle-branch block | 450 | 26 | 1.00 | 1.00 |
| RBBB | 4 | 23 | 0.78 (0.21–2.83) | 0.87 (0.24–3.18) |
| LBBB | 11 | 121 | 4.76 (2.17–10.46) | 4.22 (1.90–9.34) |
| High-degree atrioventricular block | ||||
| No bundle-branch block | 82 | 5 | 1.00 | 1.00 |
| RBBB | 3 | 18 | 3.15 (0.69–14.34) | 3.64 (0.79–16.72) |
| LBBB | 7 | 80 | 17.77 (6.42–49.20) | 12.89 (4.13–40.24) |
| Pacemaker | ||||
| No bundle-branch block | 144 | 8 | 1.00 | 1.00 |
| RBBB | 6 | 36 | 3.91 (1.33–11.45) | 4.45 (1.51–13.15) |
| LBBB | 7 | 81 | 11.73 (4.32–31.85) | 8.48 (2.85–25.30) |
| Atrial fibrillation | ||||
| No bundle-branch block | 873 | 53 | 1.00 | 1.00 |
| RBBB | 12 | 72 | 1.27 (0.60–2.68) | 1.33 (0.62–2.80) |
| LBBB | 9 | 105 | 2.39 (1.01–5.68) | 1.85 (0.74–4.63) |
| Heart failure | ||||
| No bundle-branch block | 1032 | 62 | 1.00 | 1.00 |
| RBBB | 14 | 84 | 1.22 (0.61–2.43) | 1.33 (0.66–2.66) |
| LBBB | 15 | 177 | 3.54 (1.81–6.92) | 3.26 (1.66–6.41) |
| Aortic stenosis | ||||
| No bundle-branch block | 178 | 10 | 1.00 | 1.00 |
| RBBB | 2 | 12 | 1.00 (0.16–6.29) | 1.10 (0.18–6.92) |
| LBBB | 5 | 58 | 5.98 (1.86–19.26) | 4.33 (1.16–16.13) |
| All-cause mortality | ||||
| No bundle-branch block | 3219 | 190 | 1.00 | 1.00 |
| RBBB | 29 | 169 | 0.80 (0.50–1.30) | 0.88 (0.54–1.42) |
| LBBB | 30 | 329 | 1.92 (1.20–3.08) | 1.85 (1.15–2.97) |
aAdjustment for age, systolic blood pressure, serum cholesterol, body mass index, family history of myocardial infarction, treatment for hypertension, angina, diabetes, smoking, and leisure time physical activity.
Cardiac end-points and hazard ratios by the absence or presence of right- or left-bundle-branch block in 5719 men without angina or dyspnoea at baseline in 1970–1972
| . | Number of cases . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|
| Non-fatal myocardial infarction | |||
| No bundle-branch block | 761 | 1.00 | 1.00 |
| RBBB | 9 | 1.02 (0.43–2.43) | 1.08 (0.45–2.57) |
| LBBB | 6 | 1.68 (0.58–4.84) | 1.59 (0.551–4.58) |
| Acute myocardial infarction | |||
| No bundle-branch block | 1199 | 1.00 | 1.00 |
| RBBB | 11 | 0.78 (0.36–1.70) | 0.81 (0.37–1.77) |
| LBBB | 14 | 2.58 (1.29–5.15) | 2.50 (1.245–5.02) |
| All coronary deaths | |||
| No bundle-branch block | 614 | 1.00 | 1.00 |
| RBBB | 3 | 0.38 (0.09–1.69) | 0.39 (0.09–1.72) |
| LBBB | 11 | 3.96 (1.81–8.67) | 3.95 (1.80–8.70) |
| Out-of-hospital coronary deaths | |||
| No bundle-branch block | 315 | 1.00 | 1.00 |
| RBBB | 2 | 0.49 (0.08–3.07) | 0.50 (0.08–3.14) |
| LBBB | 8 | 5.62 (2.23–14.14) | 5.21 (2.06–13.21) |
| High-degree atrioventricular block | |||
| No bundle-branch block | 56 | 1.00 | 1.00 |
| RBBB | 2 | 2.74 (0.43–17.51) | 2.99 (0.46–19.34) |
| LBBB | 5 | 21.83 (6.54–72.90) | 15.92 (3.93–64.50) |
| Pacemaker | |||
| No bundle-branch block | 96 | 1.00 | 1.00 |
| RBBB | 5 | 4.40 (1.35–14.38) | 4.57 (1.39–15.04) |
| LBBB | 5 | 14.74 (4.51-48.15) | 10.98 (2.87-41.91) |
| Atrial fibrillation | |||
| No bundle-branch block | 645 | 1.00 | 1.00 |
| RBBB | 10 | 1.27 (0.56–2.90) | 1.31 (0.58–2.99) |
| LBBB | 5 | 1.96 (0.62–6.22) | 1.31 (0.36–4.77) |
| Heart failure | |||
| No bundle-branch block | 730 | 1.00 | 1.00 |
| RBBB | 9 | 0.98 (0.41–2.32) | 1.00 (0.42–2.39) |
| LBBB | 10 | 3.77 (1.66–8.56) | 3.73 (1.63–8.51) |
| Aortic stenosis | |||
| No bundle-branch block | 127 | 1.00 | 1.00 |
| RBBB | 1 | 0.61 (0.05–8.17) | 0.62 (0.05–8.28) |
| LBBB | 3 | 5.82 (1.29–26.21) | 3.77 (0.59–24.00) |
| All-cause mortality | |||
| No bundle-branch block | 2279 | 1.00 | 1.00 |
| RBBB | 22 | 0.76 (0.44–1.33) | 0.80 (0.46–1.39) |
| LBBB | 17 | 1.70 (0.91–3.19) | 1.74 (0.93–3.27) |
| . | Number of cases . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|
| Non-fatal myocardial infarction | |||
| No bundle-branch block | 761 | 1.00 | 1.00 |
| RBBB | 9 | 1.02 (0.43–2.43) | 1.08 (0.45–2.57) |
| LBBB | 6 | 1.68 (0.58–4.84) | 1.59 (0.551–4.58) |
| Acute myocardial infarction | |||
| No bundle-branch block | 1199 | 1.00 | 1.00 |
| RBBB | 11 | 0.78 (0.36–1.70) | 0.81 (0.37–1.77) |
| LBBB | 14 | 2.58 (1.29–5.15) | 2.50 (1.245–5.02) |
| All coronary deaths | |||
| No bundle-branch block | 614 | 1.00 | 1.00 |
| RBBB | 3 | 0.38 (0.09–1.69) | 0.39 (0.09–1.72) |
| LBBB | 11 | 3.96 (1.81–8.67) | 3.95 (1.80–8.70) |
| Out-of-hospital coronary deaths | |||
| No bundle-branch block | 315 | 1.00 | 1.00 |
| RBBB | 2 | 0.49 (0.08–3.07) | 0.50 (0.08–3.14) |
| LBBB | 8 | 5.62 (2.23–14.14) | 5.21 (2.06–13.21) |
| High-degree atrioventricular block | |||
| No bundle-branch block | 56 | 1.00 | 1.00 |
| RBBB | 2 | 2.74 (0.43–17.51) | 2.99 (0.46–19.34) |
| LBBB | 5 | 21.83 (6.54–72.90) | 15.92 (3.93–64.50) |
| Pacemaker | |||
| No bundle-branch block | 96 | 1.00 | 1.00 |
| RBBB | 5 | 4.40 (1.35–14.38) | 4.57 (1.39–15.04) |
| LBBB | 5 | 14.74 (4.51-48.15) | 10.98 (2.87-41.91) |
| Atrial fibrillation | |||
| No bundle-branch block | 645 | 1.00 | 1.00 |
| RBBB | 10 | 1.27 (0.56–2.90) | 1.31 (0.58–2.99) |
| LBBB | 5 | 1.96 (0.62–6.22) | 1.31 (0.36–4.77) |
| Heart failure | |||
| No bundle-branch block | 730 | 1.00 | 1.00 |
| RBBB | 9 | 0.98 (0.41–2.32) | 1.00 (0.42–2.39) |
| LBBB | 10 | 3.77 (1.66–8.56) | 3.73 (1.63–8.51) |
| Aortic stenosis | |||
| No bundle-branch block | 127 | 1.00 | 1.00 |
| RBBB | 1 | 0.61 (0.05–8.17) | 0.62 (0.05–8.28) |
| LBBB | 3 | 5.82 (1.29–26.21) | 3.77 (0.59–24.00) |
| All-cause mortality | |||
| No bundle-branch block | 2279 | 1.00 | 1.00 |
| RBBB | 22 | 0.76 (0.44–1.33) | 0.80 (0.46–1.39) |
| LBBB | 17 | 1.70 (0.91–3.19) | 1.74 (0.93–3.27) |
5628 men had no BBB, 60 men had RBBB, and 31 men had LBBB at baseline
aAdjustment for age, systolic blood pressure, serum cholesterol, body mass index, family history of myocardial infarction, treatment for hypertension, angina, diabetes, smoking, and leisure time physical activity.
Cardiac end-points and hazard ratios by the absence or presence of right- or left-bundle-branch block in 5719 men without angina or dyspnoea at baseline in 1970–1972
| . | Number of cases . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|
| Non-fatal myocardial infarction | |||
| No bundle-branch block | 761 | 1.00 | 1.00 |
| RBBB | 9 | 1.02 (0.43–2.43) | 1.08 (0.45–2.57) |
| LBBB | 6 | 1.68 (0.58–4.84) | 1.59 (0.551–4.58) |
| Acute myocardial infarction | |||
| No bundle-branch block | 1199 | 1.00 | 1.00 |
| RBBB | 11 | 0.78 (0.36–1.70) | 0.81 (0.37–1.77) |
| LBBB | 14 | 2.58 (1.29–5.15) | 2.50 (1.245–5.02) |
| All coronary deaths | |||
| No bundle-branch block | 614 | 1.00 | 1.00 |
| RBBB | 3 | 0.38 (0.09–1.69) | 0.39 (0.09–1.72) |
| LBBB | 11 | 3.96 (1.81–8.67) | 3.95 (1.80–8.70) |
| Out-of-hospital coronary deaths | |||
| No bundle-branch block | 315 | 1.00 | 1.00 |
| RBBB | 2 | 0.49 (0.08–3.07) | 0.50 (0.08–3.14) |
| LBBB | 8 | 5.62 (2.23–14.14) | 5.21 (2.06–13.21) |
| High-degree atrioventricular block | |||
| No bundle-branch block | 56 | 1.00 | 1.00 |
| RBBB | 2 | 2.74 (0.43–17.51) | 2.99 (0.46–19.34) |
| LBBB | 5 | 21.83 (6.54–72.90) | 15.92 (3.93–64.50) |
| Pacemaker | |||
| No bundle-branch block | 96 | 1.00 | 1.00 |
| RBBB | 5 | 4.40 (1.35–14.38) | 4.57 (1.39–15.04) |
| LBBB | 5 | 14.74 (4.51-48.15) | 10.98 (2.87-41.91) |
| Atrial fibrillation | |||
| No bundle-branch block | 645 | 1.00 | 1.00 |
| RBBB | 10 | 1.27 (0.56–2.90) | 1.31 (0.58–2.99) |
| LBBB | 5 | 1.96 (0.62–6.22) | 1.31 (0.36–4.77) |
| Heart failure | |||
| No bundle-branch block | 730 | 1.00 | 1.00 |
| RBBB | 9 | 0.98 (0.41–2.32) | 1.00 (0.42–2.39) |
| LBBB | 10 | 3.77 (1.66–8.56) | 3.73 (1.63–8.51) |
| Aortic stenosis | |||
| No bundle-branch block | 127 | 1.00 | 1.00 |
| RBBB | 1 | 0.61 (0.05–8.17) | 0.62 (0.05–8.28) |
| LBBB | 3 | 5.82 (1.29–26.21) | 3.77 (0.59–24.00) |
| All-cause mortality | |||
| No bundle-branch block | 2279 | 1.00 | 1.00 |
| RBBB | 22 | 0.76 (0.44–1.33) | 0.80 (0.46–1.39) |
| LBBB | 17 | 1.70 (0.91–3.19) | 1.74 (0.93–3.27) |
| . | Number of cases . | Age-adjusted hazard ratios (99% confidence interval) . | Multiple-adjusteda hazard ratios (99% confidence interval) . |
|---|---|---|---|
| Non-fatal myocardial infarction | |||
| No bundle-branch block | 761 | 1.00 | 1.00 |
| RBBB | 9 | 1.02 (0.43–2.43) | 1.08 (0.45–2.57) |
| LBBB | 6 | 1.68 (0.58–4.84) | 1.59 (0.551–4.58) |
| Acute myocardial infarction | |||
| No bundle-branch block | 1199 | 1.00 | 1.00 |
| RBBB | 11 | 0.78 (0.36–1.70) | 0.81 (0.37–1.77) |
| LBBB | 14 | 2.58 (1.29–5.15) | 2.50 (1.245–5.02) |
| All coronary deaths | |||
| No bundle-branch block | 614 | 1.00 | 1.00 |
| RBBB | 3 | 0.38 (0.09–1.69) | 0.39 (0.09–1.72) |
| LBBB | 11 | 3.96 (1.81–8.67) | 3.95 (1.80–8.70) |
| Out-of-hospital coronary deaths | |||
| No bundle-branch block | 315 | 1.00 | 1.00 |
| RBBB | 2 | 0.49 (0.08–3.07) | 0.50 (0.08–3.14) |
| LBBB | 8 | 5.62 (2.23–14.14) | 5.21 (2.06–13.21) |
| High-degree atrioventricular block | |||
| No bundle-branch block | 56 | 1.00 | 1.00 |
| RBBB | 2 | 2.74 (0.43–17.51) | 2.99 (0.46–19.34) |
| LBBB | 5 | 21.83 (6.54–72.90) | 15.92 (3.93–64.50) |
| Pacemaker | |||
| No bundle-branch block | 96 | 1.00 | 1.00 |
| RBBB | 5 | 4.40 (1.35–14.38) | 4.57 (1.39–15.04) |
| LBBB | 5 | 14.74 (4.51-48.15) | 10.98 (2.87-41.91) |
| Atrial fibrillation | |||
| No bundle-branch block | 645 | 1.00 | 1.00 |
| RBBB | 10 | 1.27 (0.56–2.90) | 1.31 (0.58–2.99) |
| LBBB | 5 | 1.96 (0.62–6.22) | 1.31 (0.36–4.77) |
| Heart failure | |||
| No bundle-branch block | 730 | 1.00 | 1.00 |
| RBBB | 9 | 0.98 (0.41–2.32) | 1.00 (0.42–2.39) |
| LBBB | 10 | 3.77 (1.66–8.56) | 3.73 (1.63–8.51) |
| Aortic stenosis | |||
| No bundle-branch block | 127 | 1.00 | 1.00 |
| RBBB | 1 | 0.61 (0.05–8.17) | 0.62 (0.05–8.28) |
| LBBB | 3 | 5.82 (1.29–26.21) | 3.77 (0.59–24.00) |
| All-cause mortality | |||
| No bundle-branch block | 2279 | 1.00 | 1.00 |
| RBBB | 22 | 0.76 (0.44–1.33) | 0.80 (0.46–1.39) |
| LBBB | 17 | 1.70 (0.91–3.19) | 1.74 (0.93–3.27) |
5628 men had no BBB, 60 men had RBBB, and 31 men had LBBB at baseline
aAdjustment for age, systolic blood pressure, serum cholesterol, body mass index, family history of myocardial infarction, treatment for hypertension, angina, diabetes, smoking, and leisure time physical activity.
References
McAnulty JH, Kauffmann S, Murphy E, Kassebaum DG, Rahimtoola SH. Survival in patients with intraventricular conduction defects.
McAnulty JH, Rahimtoola SH, Murphy ES, Kauffman S, Ritzmann LW, Kanarek J, DeMots H. A prospective study of sudden death in ‘high-risk’ bundle-branch block.
McAnulty JH, Rahimtoola SH, Murphy E, DeMots H, Ritzmann L, Kanarek PE, Kauffman S. Natural history of ‘high-risk’ bundle-branch block.
Johnson RP, Messer AL, Shreenivas, White PD. Prognosis in bundle-branch block. II. Factors influencing the survival period in left bundle-branch block.
Messer AL, Johnson RP, Shreenivas, White PD. Prognosis in bundle-branch block. III. A comparison of right and left bundle-branch block with a note on the relative incidence of each.
Scanlon PJ, Pryor R, Blount GS. Right bundle-branch block associated with left superior or inferior intraventricular block.
Shreenivas, Messer AL, Johnson RP, White PD. Prognosis in bundle-branch block. I. Factors influencing the survival period in right bundle-branch block.
Rotman M, Triebwasser JH. A clinical and follow-up study of right and left bundle-branch block.
Fahy GJ, Pinski SL, Miller DP, McCabe N, Pye C, Walsh MJ, Robinson K. Natural history of isolated bundle-branch block.
Rodstein M, Gubner R, Mills JPJ, Lovell JF, Ungerleider HE. Mortality study in bundle-branch block.
Eriksson P, Hansson PO, Eriksson H, Dellborg M. Bundle-branch block in a general male population: the study of men born 1913.
Schneider JF, Thomas HE, Sorlie P, Kreger BE, McNamara PM, Kannel WB. Comparative features of newly acquired left and right bundle-branch block.
Hardarson T, Arnarson A, Eliasson GJ, Palsson K, Eyjolfsson K, Sigfusson N. Left bundle-branch block: prevalence, incidence, follow-up and outcome.
Freedman RA, Alderman EL, Sheffield LT, Saporito M, Fisher LD. Bundle-branch block in patients with chronic coronary artery disease: angiographic correlates and prognostic significance. Coronary Artery Surgery Study (CASS).
Col JJ, Weinberg SL. The incidence and mortality of intraventricular conduction defects in acute myocardial infarction.
Newby KH, Pisano E, Krucoff MW, Green C, Natale A. Incidence and clinical relevance of the occurrence of bundle-branch block in patients treated with thrombolytic therapy.
Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of over 1000 patients.
Scheinmann MM, Peters W, Sauvè MJ, Desai J, Abbot JA, Cogan J, Wohl B, Williams K. Value of the H–Q interval in patients with bundle-branch block and the role of prophylactic permanent pacing.
Peters RW, Scheinmann MM, Modin C, O'Young J, Somelofski CA, Mies C. Prophylactic permanent pacemakers for patients with chronic bundle-branch block.
Wilhelmsen L, Berglund G, Elmfeldt D, Tibblin G, Wedel H, Pennert K, Vedin A, Wilhelemsson C, Werko L. The multifactor primary prevention trial in Göteborg, Sweden.
Wilhelmsen L, Rosengren A, Eriksson H, Lappas G. Heart failure in the general population of men—morbidity, risk factors and prognosis.
Elmfeldt D, Wilhelmsen L, Tibblin G, Vedin JA, Wilhelmsson CE, Bengtsson C. Registration of myocardial infarction in the city of Göteborg, Sweden.
Froelicher VF, Thompson AJ, Wolthuis R, Fuchs R, Balusek R, Longo MR, Triebwasser JH, Lancaster MC. Angiographic findings in asymptomatic aircrewmen with electrocardiographic abnormalities.
Haft JI, DeMaio SJ, Bartoszyk OB. Coronary arteriographic findings in symptomatic right bundle branch block.
Pièrard LA, Dubois C, Albert A, Smeets JP, Kulbertus HE. Prediction of mortality after myocardial infarction by simple clinical variables recorded during hospitalization.
Hindman MC, Wagner SG, Jaro M, Atkins JM, Scheinman MM, DeSanctis RW, Hutter AH, Yeatman L, Rubenfire M, Pujura C, Rubin M, Morris JJ. The clinical significance of bundle branch block complicating acute myocardial infarction.
Sgarbossa EB, Pinski SL, Topol EJ, Califf RM, Barbagelata A, Goodman SG, Gates KB, Granger CB, Miller DP, Underwood DA, Wagner GS. Acute myocardial infarction and complete bundle branch block at hospital admission: clinical characteristics and outcome in the thrombolytic era.
Dubois C, Pièrard L, Smeets JP, Foidart G, Legrand V, Kulbertus HE. Short- and long-term prognostic importance of complete bundle-branch block complicating acute myocardial infarction.
Lie KI, Liem KL, Schuilenburg RM, David GK, Durrer D. Early identification of patients developing late in-hospital ventricular fibrillation after discharge from the coronary care unit.
Brezins M, Elyassov S, Elimelech I, Roguin N. Comparison of patients with acute myocardial infarction with and without ventricular fibrillation.
Dhingra RC, Palileo E, Strasberg B, Swiryn S, Bauernfeind RA, Wyndham CR, Rosen KM. Significance of the HV interval in 517 patients with chronic bifascicular block.
Zehender M, Buchner C, Meinertz T, Just H. Prevalence, circumstances, mechanisms and risk stratification of sudden cardiac death in unipolar single chamber ventricular pacing.
Norris RM, Mercer CJ, Croxson MS. Conduction disturbances due to anteroseptal myocardial infarction and their treatment by endocardial pacing.