Abstract
Background: There is growing evidence that ergot dopamine agonists may induce cardiac valve regurgitation (CVR) in persons with Parkinson’s disease. It is unclear whether the CVR risk is increased with ergot-dopamine agonist use in persons with hyperprolactinaemia, in whom the dose is much lower.
Objective: The aim of the study was to explore the association between different dopamine agonists and CVR in patients with Parkinson’s disease or hyperprolactinaemia.
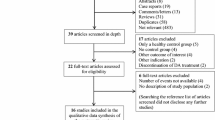
Design: Nested case-control studies conducted separately in cohorts of Parkinson’s disease and hyperprolactinaemia patients. Cases were patients who developed newly diagnosed CVR. Controls were CVR-free patients from the same cohorts and were matched to cases by age, sex, database and calendar year.
Setting and Patients: Study patients were identified from over 4.5 million persons in The Health Improvement Network (THIN; UK), Health Search (Italy), and Integrated Primary Care Information (IPCI; the Netherlands) general practice databases in the years 1996–2007. The Parkinson’s disease cohort included new users of dopamine agonists or levodopa, while the hyperprolactinaemia cohort included new users or non-users of dopamine agonists.
Main Outcome Measure: Risk of newly diagnosed CVR with dopamine agonist use compared with levodopa use in the Parkinson’s disease cohort, and dopamine agonist-naïve patients in the hyperprolactinaemia cohort.
Results: In the Parkinson’s disease cohort (7893 dopamine agonist users, 11 766 levodopa users), 85 incident CVR cases were identified. Increased CVR risk was observed for ergot dopamine agonists (adjusted OR [ORadj] 3.82; 95% CI 2.14, 6.81), but not for non-ergot dopamine agonists (ORadj 1.20; 95% CI 0.63, 2.29).
In the hyperprolactinaemia cohort (6740 dopamine agonist users and 14299 dopamine agonist-naïve patients), 37 CVR cases were identified during a mean follow-up of 4.5 years and 3.5 years for new users and non-users of dopamine agonists, respectively. However, no association with ever use of ergot dopamine agonists was observed (ORadj 0.47; 95% CI 0.20,1.19).
Conclusion: Ergot-derived dopamine agonists are associated with an increased risk of CVR in Parkinson’s disease but not in hyperprolactinaemia patients.





Similar content being viewed by others
References
Kvernmo T, Hartter S, Burger E. A review of the receptor-binding and pharmacokinetic properties of dopamine agonists. Clin Ther 2006; 28: 1065–78
Goetz CG, Poewe W, Rascol O, et al. Evidence-based medical review update: pharmacological and surgical treatments of Parkinson’s disease: 2001 to 2004. Mov Disord 2005; 20: 523–39
Horvath J, Fross RD, Kleiner-Fisman G, et al. Severe multivalvular heart disease: a new complication of the ergot derivative dopamine agonists. Mov Disord 2004; 19: 656–62
Pritchett AM, Morrison JF, Edwards WD, et al. Valvular heart disease in patients taking pergolide. Mayo Clin Proc 2002; 77: 1280–6
Van Camp G, Flamez A, Cosyns B, et al. Heart valvular disease in patients with Parkinson’s disease treated with high-dose pergolide. Neurology 2003; 61: 859–61
Pinero A, Marcos-Alberca P, Fortes J. Cabergoline-related severe restrictive mitral regurgitation. N Engl J Med 2005; 353: 1976–7
Bhattacharyya S, Schapira AH, Mikhailidis DP, et al. Drug-induced fibrotic valvular heart disease. Lancet 2009; 374: 577–85
Tan LC, Ng KK, Au WL, et al. Bromocriptine use and the risk of valvular heart disease. Mov Disord 2009; 24: 344–9
Zanettini R, Antonini A, Gatto G, et al. Valvular heart disease and the use of dopamine agonists for Parkinson’s disease. N Engl J Med 2007; 356: 39–46
Simonis G, Fuhrmann JT, Strasser RH. Meta-analysis of heart valve abnormalities in Parkinson’s disease patients treated with dopamine agonists. Mov Disord 2007; 22: 1936–42
Schade R, Andersohn F, Suissa S, et al. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 2007; 356: 29–38
Food and Drug Administration. Withdrawal of Parkinson’s treatment: pergolide. April 17, 2007 [online]. Available from URL: http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048819.htm [Accessed 2011 Feb 15]
European Medicines Agency. Scientific conclusions and grounds for amendment of the summaries of product characteristics and package leaflets of cabergoline presented by the EMA [online]. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Ergot_derived_dopamine_agonists_31/WC500011459.pdf [Accessed 2011 Feb 15]
Klibanski A. Clinical practice: prolactinomas. N Engl J Med 2010; 362: 1219–26
Colao A, Galderisi M, Di Sarno A, et al. Increased prevalence of tricuspid regurgitation in patients with prolactinomas chronically treated with cabergoline. J Clin Endocrinol Metab 2008; 93: 3777–84
Bogazzi F, Buralli S, Manetti L, et al. Treatment with low doses of cabergoline is not associated with increased prevalence of cardiac valve regurgitation in patients with hyperprolactinaemia. Int J Clin Pract 2008; 62: 1864–9
Vallette S, Serri K, Rivera J, et al. Long-term cabergoline therapy is not associated with valvular heart disease in patients with prolactinomas. Pituitary 2009; 12: 153–7
Herring N, Szmigielski C, Becher H, et al. Valvular heart disease and the use of cabergoline for the treatment of prolactinoma. Clin Endocrinol (Oxf) 2009; 70: 104–8
Nachtigall LB, Valassi E, Lo J, et al. Gender effects on cardiac valvular function in hyperprolactinaemic patients receiving cabergoline: a retrospective study. Clin Endocrinol (Oxf) 2010; 72: 53–8
Kars M, Delgado V, Holman ER, et al. Aortic valve calcification and mild tricuspid regurgitation but no clinical heart disease after 8 years of dopamine agonist therapy for prolactinoma. J Clin Endocrinol Metab 2008; 93: 3348–56
Wakil A, Rigby AS, Clark AL, et al. Low dose cabergoline for hyperprolactinaemia is not associated with clinically significant valvular heart disease. Eur J Endocrinol 2008; 159: R11–4
Lancellotti P, Livadariu E, Markov M, et al. Cabergoline and the risk of valvular lesions in endocrine disease. Eur J Endocrinol 2008; 159: 1–5
Devin JK, Lakhani VT, Byrd 3rd BF, et al. Prevalence of valvular heart disease in a cohort of patients taking cabergoline for management of hyperprolactinemia. Endocr Pract 2008; 14: 672–7
Lafeber M, Stades A, Valk G, et al. Absence of major fibrotic adverse events in hyperprolactinemic patients treated with cabergoline. Eur J Endocrinol 2010; 162: 667–75
Tan T, Cabrita IZ, Hensman D, et al. Assessment of cardiac valve dysfunction in patients receiving cabergoline treatment for hyperprolactinaemia. Clin Endocrinol (Oxf) 2010; 73: 369–74
Lewis JD, Schinnar R, Bilker WB, et al. Validation studies of the health improvement network (THIN) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf 2007; 16: 393–401
Cricelli C, Mazzaglia G, Samani F, et al. Prevalence estimates for chronic diseases in Italy: exploring the differences between self-report and primary care databases. J Public Health Med 2003; 25: 254–7
van der Lei J, Duisterhout JS, Westerhof HP, et al. The introduction of computer-based patient records in The Netherlands. Ann Intern Med 1993; 119: 1036–41
Richardson DB. An incidence density sampling program for nested case-control analyses. Occup Environ Med 2004; 61: e59
Committee on Safety of Medicines. Pergolide (Celance) and cardiac valvulopathy. Current problems in pharmacovigilance bulletin. Vol. 29. London: Medicines and Healthcare Products Regulatory Agency, 2003: 7
Vallette S, Serri K, Serri O. Cabergoline therapy for prolactinomas: is valvular heart disease a real safety concern? Expert Rev Cardiovasc Ther 2010; 8: 49–54
Yamamoto M, Uesugi T, Nakayama T. Dopamine agonists and cardiac valvulopathy in Parkinson disease: a case-control study. Neurology 2006; 67: 1225–9
Peralta C, Wolf E, Alber H, et al. Valvular heart disease in Parkinson’s disease vs. controls: an echocardiographic study. Mov Disord 2006; 21: 1109–13
Zanettini R, Antonini A, Gatto G, et al. Regression of cardiac valvulopathy related to ergot-derived dopamine agonists. Cardiovasc Ther. Epub 2010 Jun 11
Van Camp G, Flamez A, Cosyns B, et al. Treatment of Parkinson’s disease with pergolide and relation to restrictive valvular heart disease. Lancet 2004; 363: 1179–83
Acknowledgements
C. de Luise and D. Ross are employees of Pfizer and own Pfizer stock. As an employee of Erasmus MC and project leader of the IPCI database, M.C.J.M. Sturkenboom has been involved in studies that were contracted by various pharmaceutical companies. Research grants have been received from Pfizer, Merck, Johnson & Johnson, Amgen, Roche, GlaxoSmithKline, Boehringer, Yamanouchi and Altana. M.C.J.M. Sturkenboom has been a consultant to Pfizer on issues not related to this paper. G. van Camp received preliminary funds for the study “Effect of chronic administration of candidate 5HT2b agonist/antagonist on the cardiac valves in an in vivo rat model: evaluation with echocardiography and pathology”, which was then subsequently cancelled by Pfizer. G. van Camp has also been a consultant for AstraZeneca and Pfizer, has received honoraria from AstraZeneca, Pfizer, GE, Philips, Boston Scientific and Biotronic, and has received research grants from AstraZeneca and Pfizer. A. Colao received grants from Pfizer for research projects in neuroendocrinology. Ron Herings is an employee of the PHARMO Institute. This research institute performs financially supported studies for several pharmaceutical companies, including Pfizer. R. Schade has been a consultant to Axxonis Pharma AG and has received grants from Schering AG. J. Dieleman has been involved in studies conducted with grants from Pfizer, Boehringer, Lilly and AstraZeneca. G. Trifirò, E. van Soest, K. Verhamme, G. Mazzaglia, E. Brusselle, W. Haverkamp, R. Zanettini and M. Mokhles have no conflicts of interest to declare.
G. Brusselle, A. Colao, W. Haverkamp, R. Schade, G. van Camp, and R. Zanettini were all members of the Scientific Advisory Board of the project resulting in this paper. G. Trifirò had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; G. Trifirò, M. Sturkenboom, K. Verhamme and C. de Luise played a major role in the study concept and design; analysis and interpretation of data, as well as drafting of the manuscript, was mainly performed by G. Trifirò, M. Sturkenboom, M. Mokhles, J. Dieleman, E. van Soest and G. Mazzaglia; all the authors carried out a critical revision of the manuscript for important intellectual content and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trifirò, G., Mokhles, M.M., Dieleman, J.P. et al. Risk of Cardiac Valve Regurgitation with Dopamine Agonist use in Parkinson’s Disease and Hyperprolactinaemia. Drug Saf 35, 159–171 (2012). https://doi.org/10.2165/11594940-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11594940-000000000-00000